During a recent NASHP webinar, experts and state administrators spoke about the benefits of POLST as well as promising practices and lessons learned from West Virginia and Louisiana.
A POLST is a portable medical order that communicates treatment goals and preferences for people with serious illness or advanced frailty. The use of POLST can help to ensure that patients treatment preferences are respected in critical clinical situations and to avoid unwanted treatments if patients cannot speak for themselves during a medical crisis. A 2020 JAMA study found that, while many patients still received care that did not reflect their POLST order, treatment-limiting POLSTs were associated with significantly lower rates of intensive care unit (ICU) admission compared with full-treatment POLSTs.
End of life care is essential. Pain and paperwork are overwhelming when trying to grant your loved ones wishes, said Delegate Danielle Walker from West Virginia about POLST.
States adopt POLST as part of a range of efforts to strengthen person-centered care and advance care planning for people with serious illness. While advance directives are advisable for all adults to help direct their care should they become unable to do so, POLST is specifically for people with serious illness or frailty. POLST provides specific medical orders regarding health care and end of life decisions compared to the general wishes described in advance directives and more options than Do Not Resuscitate orders.
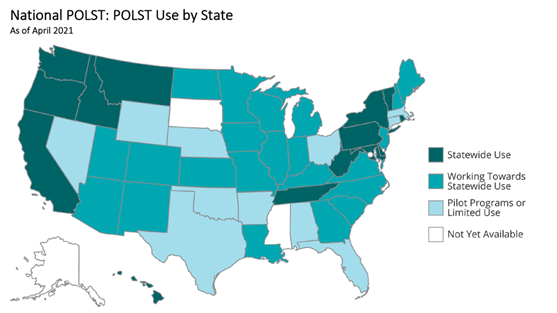
State Use of POLST
In its 2015 seminal report, Dying in America, the National Academy recommended that states develop and implement POLST in accordance with nationally standardized core requirements. National POLST is working toward the adoption within states of a National POLST form to support portability and consistency across states.
While most states use POLST forms, the forms may not be available to all people who could benefit, or may not be standard practice throughout hospitals, nursing homes, and hospices across the state.
What States Can Do to Promote POLST?
Support state POLST Programs. All states have adopted a statewide POLST form and most have a coalition or task force supporting education efforts to ensure appropriate use of POLST.
Consider Adopting or Adapting the National POLST Form. States have already adopted a single statewide form to create a standardized document, but they can also adopt the National POLST form for portability and consistency across states. Seven states–Arizona, Maine, New Hampshire, Iowa, Alabama, West Virginia, and Alaska–either use or have adapted the National POLST form. In West Virginia, for example, the state legislature enacted the Health Care Decisions Act in 2000 to ensure that a patient’s right to self-determination in health care decisions be communicated and protected. In 2002, the Act was amended to include the West Virginia Physician Orders for Scope of Treatment form, now referred to simply as POST, which is used statewide.
Develop a comprehensive POLST registry. Electronic registries enable emergency medical service personnel and medical providers statewide to access the treatment preferences of anyone who has completed a POLST form. The West Virginia Center for End-of-Life Care was established with support from the legislature and houses the states e-Directive registry. The registry provides access to POLST and other advance care planning information in a medical crisis for example, while emergency medical personnel are in route. Health care providers have 24/7 online access through West Virginia Health Information Networkthe states Health Information Exchangewhich enables the secure electronic exchange of patient health information among providers. This information is password protected and HIPAA compliant. National POLST tracks the states with registries and provides information for those considering one.
Conduct outreach and education. States have emphasized the importance of education and outreach to garner legislative support for statewide adoption of POLST and implementation of a registry. The Louisiana Health Care Quality Forum, a private, nonprofit organization, administers the statewide Louisiana Physician Order for Scope of Treatment (LaPOST) Registry. The Forum educates physicians, health care professionals in nursing homes and assisted living, emergency medical service personnel, and the general public. Currently, the Forum is working to allow providers across settings in the state to electronically complete, store, and access patients end-of life wishes.
Learn from other states and get involved with National POLST. There is a wealth of state experience with medical order forms, which provides important lessons learned. For example, the Louisiana legislature enacted Act 954 in 2010 to provide for the Louisiana Physician Order for Scope of Treatment (POST) program and form. Unfortunately, the legislature embedded the POST document into the statute. It is advisable to omit embedding the actual form into the legislation to allow flexibility in updating the document as new research or improved practices emerge. Legislatures can include language requiring a form and describing baseline requirements for POLST to allow for updates.
To learn more from other states about advance care planning and palliative care, NASHP hosts a Palliative Care Resource Hubfunded by a grant from The John A. Hartford Foundationthat contains a series of state policy tools and resources.




