Contact tracing is an essential strategy for curbing the spread of COVID-19. When implemented quickly, isolation of people diagnosed with COVID-19 and identification and quarantine of close contacts can effectively interrupt disease transmission and reduce spread. Faced with rapidly climbing caseloads, testing delays, and increases in community spread, states and localities have had to prioritize high-risk cases, utilize technology in new ways, and implement creative strategies to conduct case investigations, trace contacts of infected individuals, and perform follow-up.
Contact tracing works best when quick follow-up is possible, sufficient testing resources are available, and when social isolation and quarantine are possible. Due to recent case spikes, contact tracers in some states are unable to call COVID-19-positive individuals fast enough. Additionally, with some regions reaching an accelerating state of community spread, it is more difficult to determine exactly where individuals were exposed to COVID-19. In North Dakota, these issues led to a major shift in contact tracing protocols. Since October, the state has asked infected individuals to notify their close contacts and direct them to resources on the Department of Health’s website.
View NASHP’s interactive map that highlights State Approaches to Contact Tracing during the COVID-19 Pandemic.
Listen to a new Mathematica video podcast, Understanding the Variation in States COVID-19 Contact Tracing Approaches, that features NASHP staff.
Recently, other states have followed suit:
- The Maine Center for Disease Control and Prevention will make only one contact with an infected individual (instead of checking in with them periodically) to provide guidance. It will also enroll people in the program based on when their last contact with someone with COVID-19 was. That way, they will enroll people who have the highest number of days left in their 10-day quarantine period so Maine CDC can work with them as early as possible to limit exposure to others in the community. The state is also limiting its contact tracing to high-risk individuals, including those age 65 and older, health care workers, children, individuals of color, school workers, and congregate living facility residents.
- As of mid-November, Nebraska had a backlog of 2,600 people who had tested positive for COVID-19 but had not been contacted by a contact tracer. To address the backlog, the Department of Health and Human Services reduced the number of call attempts from five to two, reduced the number of interview questions, and asked individuals to call their own contacts to let them know they tested positive.
- New Hampshire began focusing on contact tracing for high-risk populations including health care workers, communities of color, and people living in group living spaces. The state is also asking health care providers to educate COVID-19-positive patients about isolation and quarantine procedures.
- Oregon has shifted tracking priorities as its case counts rise drastically to protect the states most vulnerable residents in long-term care facilities, jails, foster homes, etc. Contact tracers are still advised to perform the first two steps of tracing: interviewing new COVID-19 cases and finding their contacts and notifying them to get tested and quarantine, but they will no longer do ongoing monitoring of these groups.
- Pennsylvania is prioritizing case investigations of its most vulnerable residents, such as those in nursing homes, or cases that could lead to greater community spread.
- In Wisconsin and Wyoming, only individuals who have tested positive for COVID-19 will hear from contact tracers. Individuals are instructed to reach out to their own close contacts.
Since spring, states have shifted their approaches to contact tracing to reflect current needs. The examples above show that states are currently focused on maximizing contact tracing effectiveness by focusing on known or presumed positive cases and working to protect those at increased risk through a more targeted approach to contact tracing outreach.
Additionally, several of these states have been financing their contact tracing efforts with federal funds and there is some uncertainty about whether these funds will be renewed. With the year drawing to a close, there are competing demands for these resources as states prepare for vaccine distribution and education, and funding has likely played into decisions to cut back instead of hiring new contact tracers.
In a recent press conference, Maine CDC Director Nirav Shah, compared the need for contact tracing prioritization to a “very busy, crowded emergency room, serving first those in the highest need at their greatest moment of need.”
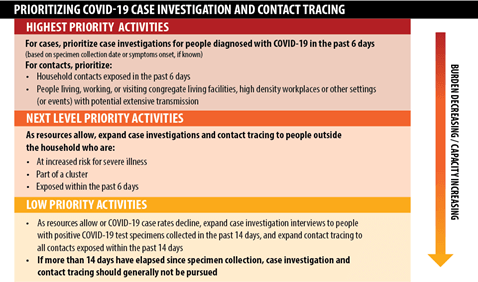
In response to state actions like the ones above, the US Centers for Disease Control and Prevention (CDC) released new guidance on Dec. 3, 2020, about how to prioritize contact tracing and case investigation in states and jurisdictions where cases are on the rise. The new directions were guided by several principles:
- Maximizing effectiveness;
- Protecting household contacts;
- Preventing outbreaks and clusters; and
- Protecting people at increased risk.
Virginia has adopted these guidelines and will join the list of states that are using contact tracing prioritization as a way to address surging cases.
States can use other strategies in their contact tracing work to maximize value, including technology. As of Dec. 1, 17 states were using the Google and Apple exposure notification technology that alerts individuals when they have been in close contact with someone who has tested positive for COVID-19. There is an increasing focus on these phone applications working across state lines as the technology becomes more standardized. In other states, technology is being used to connect people with quarantine resources – a strategy that can make contact tracing more effective.
For example, in Connecticut, a statewide software system called ContaCT monitors test results and positive cases. The ContaCT platform will identify and refer people who need support at initiation and throughout self-isolation or self-quarantine. Case workers will support people in self-isolation or self-quarantine by connecting them with state, local, and regional resources as necessary, such as food and housing.
Other states are using a range of strategies to improve the efficiency or effectiveness of their contact tracing programs in the face of rising caseloads and hospitalization rates:
- The Ohio Department of Health is updating its systems to allow local health departments to enter information about an infected person’s contacts prior to their positive test to get a better idea of where the virus is likely to spread.
- Since August, Washington, DC contact tracing efforts have included home visits for high-risk individuals who did not complete contact tracing interviews or could not be reached by contact tracers.
- North Dakota, South Dakota, and Vermont have recently revived their partnerships with the National Guard to help with elements of contact tracing and case investigation.
- In New Mexico, businesses that have had a confirmed COVID-19 case or exposure among staff can avoid a 14 day Rapid Response Closure by signing a surveillance testing and contact tracing In the document the employers must agree to conduct testing among their staff and select a COVID-19 coordinator responsible for working with the NM Department of Health on contact tracing efforts in the workplace.
- South Dakota is incorporating texting and email into their initial outreach strategy, replacing phone calls in some cases. This approach can be more automated and will allow individuals to input their own information to a secure online portal even if they are unable or unwilling to answer the phone.
Contact tracing is just one piece of the puzzle when it comes to mitigating the spread of COVID-19. Increased public education about the importance of mask wearing and social distancing, as well as increased testing and resources for effective quarantine will also be critical for curbing the spread. As COVID-19 case numbers rise and fluctuate this winter, states are expected to continue to adjust their contact tracing and case investigation strategies to meet their needs and utilize available resources. The National Academy for State Health Policy, in partnership with Mathematica, will continue to track and analyze state efforts.
Support for this work was provided by the Robert Wood Johnson Foundation. The views expressed here do not necessarily reflect the views of the foundation.

 Source:
Source: 

