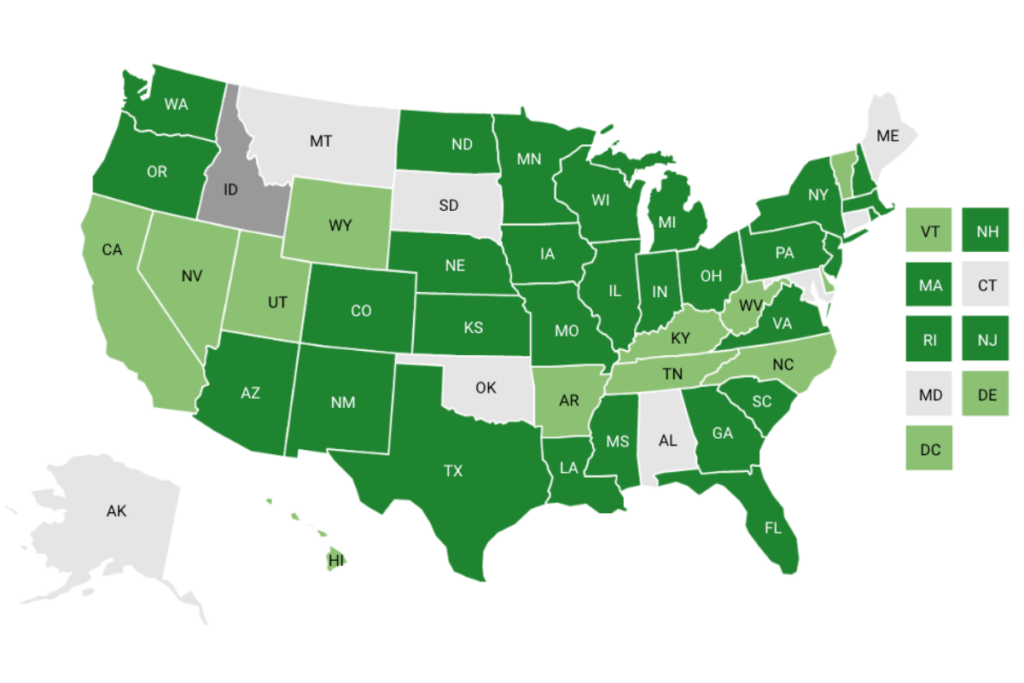
Contact tracing is an essential strategy to curb the spread of COVID-19. Across the country, states have developed, deployed, and adapted their contact tracing approaches in response to the pandemic. Reflecting changes in CDC guidance, some states have stopped conducting universal contact tracing and are focusing efforts on outbreaks and at-risk populations. NASHP and Mathematica have partnered to develop this interactive map. Click on a state to learn about its tracing program or explore the information below the map to compare states’ approaches.
Explore a Mathematica resource on the demographics, methodology, and implications for contact tracing and a Mathematica podcast, Understanding the Variation in States’ COVID-19 Contact Tracing Approaches.
In-house: State/local officials lead, hiring or recruiting volunteers as needed.
Contracting: The state contracts with a company or organization for contact tracing work/hiring.
Partnering: State leads efforts but relies on partners for training/staffing.
Suspended or shifted locally: The state-wide contact tracing program has been suspended or shifted to local health departments.
State | Model |
AL | Suspended or shifted locally. The state no longer conducts routine contact tracing. It conducts a limited number of investigations into certain population and settings. |
AK | Suspended or shifted locally. The state no longer contacts every positive case and prioritizes outbreak investigation and mitigation. |
AZ | Partnering. The CDC Foundation supports recruitment for the contact tracing workforce. The state and local health departments perform contact tracing. |
AR | Suspended or shifted locally. The state stopped universal contact tracing efforts. |
CA | Suspended or shifted locally. In June 2022 the state’s redirected COVID-19 CICT staffing support program ended. |
CO | Partnering. The state and local governments lead with support from volunteers and a partnership with a federal agency. |
CT | Partnering. The Connecticut Department of Public Health and local health departments lead the work and provide staff. |
DC | Suspended or shifted locally. As of July 2022, the city has ended its universal contact tracing program. |
DE | Partnering. The state Division of Public Health leads. NORC at the University of Chicago hires and trains contact tracers. |
FL | Suspended or shifted locally. In January 2022, the state recommended that county health departments cease contact tracing. |
GA | Partnering. The state leads the contact tracing effort with outside assistance for training and technology. |
HI | Suspended or shifted locally. |
ID | In-house. Idaho’s seven independent health districts are responsible for doing case investigations and hiring their own contact tracing staff. |
IL | Suspended or shifted locally. In June 2022, the state moved to confirmed/probable case notification only. |
IN | Suspended or shifted locally. The state conducts contact tracing for clusters or outbreaks. |
IA | Suspended or shifted locally. The state no longer contacts every positive case and prioritizes outbreaks and people at greater risk for exposure to COVID-19. |
KS | Suspended or shifted locally. The state no longer conducts case investigation and contact tracing, citing high caseloads and resistance to participation. |
KY | Suspended or shifted locally. The state no longer conducts universal contact tracing except among people at higher risk of potential exposure to COVID-19. |
LA | Suspended or shifted locally. The state is no longer conducting case investigation and contact tracing of individual cases of COVID-19 but continues to investigate COVID-19 outbreaks and cases in high-risk settings. |
ME | Suspended or shifted locally. The state no longer conducts contact tracing. |
MD | Partnering. The state is leading the effort with outside help from NORC for staffing. Local health departments are conducting contact tracing; the state Department of Health has contracted with NORC for outside assistance. |
MA | Suspended or shifted locally. The state no longer conducts universal contact tracing and residents are encouraged to use MassNotify, the state’s exposure notification app. |
MI | Suspended or shifted locally. The statewide contact tracing and individual-level case investigation effort has come to an end. Local health departments have been directed to focus contact tracing efforts on congregate settings and outbreaks. |
MN | Suspended or shifted locally. As of May 2022, the state was reportedly no longer conducting contact tracing. |
MS | In-house. led and implemented by the State Department of Health. |
MO | Suspended or shifted locally. The state recommends local contact tracing for people at greater risk for exposure to COVID-19. |
MT | Suspended or shifted locally. In May 2022, the Montana Department of Public Health and Human Services announced that local public health officials would continue to investigate COVID-19 outbreaks and cases in settings which may expose individuals at high risk for severe outcomes. |
NE | Partnering. The state is leading some of the effort while contracting with Professional Research Consultants, a health care research company. |
NV | Partnering. The state is contracting with organizations such as the University of Nevada – Reno and the University of Nevada – Las Vegas to expand local efforts. Local health departments are leading, and the state Department of Health and Human Services oversees contact tracing staffing. |
NH | Suspended or shifted locally. As of June 2021, the state no longer conducts contact tracing for exposures in community settings but does investigate suspected outbreaks. |
NJ | Suspended or shifted locally. The state is no longer contact tracing for the general population, and individuals who test positive are encouraged to get in touch with their own close contacts. Contact tracing is managed by the state Department of Health in partnership with the Public Consulting Group and New Jersey Community Contact Tracing Corps. |
NM | Contracting with Accenture to manage the contact tracing effort and set up a call center. |
NY | Suspended or shifted locally. The state is following CDC’s case investigation and contact tracing guidance, which focuses on providing information to those who tested positive most recently and those who may have close contacts in sensitive settings. |
NC | Partnering. The state is contracting with organizations to build on local efforts. The state Department of Health and Human Services is supporting and building on the efforts of local health departments. |
ND | Partnering. The state is managing the effort and working with Governor’s Office, Department of Human Services, North Dakota Information Technology, their chief health strategist, and the State University disease specialist. |
OH | Suspended or shifted locally. Local health departments are leading with support from the state Department of Health. |
OK | Suspended or shifted locally. In January 2022, the state announced it would move away from universal case investigation and contact tracing amid the omicron surge. Instead, they will focus on outbreaks and clusters in high-risk settings. |
OR | Suspended or shifted locally. As of March 2022, the state ended contact tracing and quarantine for the general population, but it continues to recommend contact tracing during investigation of high-consequence outbreaks, led by local public health authorities and supported by the state. |
PA | Contracting with the Public Consulting Group to supplement state and local contact tracing staff. |
RI | Suspended or shifted locally. In February 2022, the state began to focus case investigation and contact tracing response efforts on people who are at higher risk and outbreak detection, with the intention of shifting away from universal contact tracing. |
SC | Suspended or shifted locally. The state is leading the effort to conduct case investigations of clusters of COVID cases where there are populations in high-risk, congregate settings with potential risk for ongoing transmission. |
SD | In-house. The state is managing the workforce with supplemental support from the National Guard and the University of South Dakota. The University of South Dakota’s Community Action Response Epidemiology (CARE) team partnered with the state to provide contact tracing for the university and for the state’s tribal communities. |
TN | Suspended or shifted locally. The state and local departments of health are scaling back contact tracing. They are no longer conducting universal contact tracing and are instead focusing on high-risk settings such as nursing homes, prisons, and homeless shelters. |
TX | Suspended or shifted locally. The state does not allow funds to be used for contact tracing in the current budget. |
UT | Suspended or shifted locally. As of March 2022, the state contact tracing effort is shifting to high-risk population or large outbreaks. |
VT | Suspended or shifted locally. The state is no longer contacting every positive case and prioritizes long-term care facilities and shelters. |
VA | Suspended or shifted locally. In January 2022, the state announced that it will only conduct contact tracing in high-risk settings and in follow-up of an outbreak. |
WA | Partnering. Local health jurisdictions lead with support from the state Department of Health and its partners. |
WV | Suspended or shifted locally. As of February 2022, the state’s Department of Health and Human Resources Bureau transitioned from universal case investigations and contact tracing to targeted case investigations and outbreak investigations. |
WI | In-house. The state, local, and tribal health departments are leading contact tracing. |
WY | Suspended or shifted locally. The state is no longer attempting to reach individuals who have tested positive for COVID-19 unless they are part of a high-risk congregate settings, outbreaks and clusters of related cases, and the emergence of new variants. |
| State | Tracing Process |
| AL | As of May 2022, the Alabama Department of Public Health (ADPH) no longer conducts routine contact tracing. The state conducts a limited number of investigations into cases involving school-aged children and congregate living facilities. ADPH recommends people who test positive for COVID-19 notify their close contacts if they become ill. Local health departments can determine how case investigations and contact tracing should be implemented in each jurisdiction. |
| AK | The state follows a strategic approach of outbreak investigation and mitigation. Individuals are encouraged to notify their own close contacts, as more Alaskans rely on at-home testing that does not get reported to the state. Individuals are encouraged to call the Public Health Nursing line or their local Public Health Center for guidance on local resources, isolation, and quarantine. |
| AZ | The state conducts initial contact tracing outreach via manual calls to prioritized cases. As of February 2022, the state prioritizes cases if they are over the age of 80, school-aged kids, cases with multiple comorbidities, or are in a congregate setting. State and county health departments also send text messages and digital surveys to these prioritized groups, and contact tracers can offer advice on quarantine recommendations and guidance on local resources. Individuals are encouraged to notify their own close contacts. A close contact is defined as someone who has been within six feet of an infected person for a total of 15 minutes or more over a 24-hour period between 2 days before and 10 days after symptom onset, or test date for asymptomatic cases. Produce companies that employ migrant farmers have partnered with nonprofit health organizations to provide testing and contact tracing for their workers. Among the White Mountain Apache tribe in Arizona, contact tracing includes home visits where all members of the household are tested for COVID-19. |
| AR | The state Department of Health no longer conducts contact tracing for adults but will focus on conducting case investigations for kids and teens 18 and under. Families of new cases are contacted to collect and share information, but contact tracing is not conducted. Individuals are encouraged to familiarize themselves with the CDC’s guidelines and to notify their own close contacts in the event of a positive test result. |
| CA | In March 2022 the state health department recommended that local health jurisdictions prioritize case investigation and contact tracing efforts for high-risk individuals or settings, and to leverage automated notifications and public education and information for cases and exposed persons in the general population. In June 2022 the state’s redirected COVID-19 CICT staffing support program ended. The state continues to maintain the CalCONNECT and CA Notify systems and user support and to provide resources and support to local health jurisdictions related to CICT safety-net staffing, workforce training, and outbreak investigation consultation. Anyone within six feet of a person with COVID-19 for at least 15 minutes indoors is considered a contact. State guidance recommends the inclusion of core demographic variables (e.g., race, ethnicity, preferred language) on all case investigation and contact tracing forms to inform more diversified outreach. Individuals who receive a positive result from a CareStart at-home test can report the results to the state using a QR code or via an online form. They are also encouraged to contact their primary care provider, alert close contacts, and isolate for five days. As of April 2022, the state no longer recommends quarantine for people who were exposed to COVID-19 but do not have symptoms. As of July 2022, Los Angeles County is shifting resources toward vaccines and therapeutics and targeting contact tracing toward specific high-risk demographics and zip codes. |
| CO | The state recommends that individuals who test positive for COVID-19 let their contacts know that they may have been exposed. The state health department may contact those with positive test results to collect information about exposures and give information about preventing transmission to others. As of January 2022, the state prioritizes case investigation and contact tracing activities to higher-risk settings. As of January 2022, with increased use of at-home testing, the state encourages individuals to report positive results to the health department online or by phone to allow for contact tracing. Individuals who test positive are also recommended to stay home, isolate, and notify close contacts. A close contact is considered anyone who spent time in close proximity to or had direct contact with someone while they were infectious. |
| CT | The state conducts initial contact tracing outreach via automated text messages or emails and manual phone calls to those who do not respond to the text messages or emails. Individuals are also encouraged to alert their own close contacts of a positive test result. The state uses a software system called ContaCT for monitoring test results and positive cases. ContaCT identifies and refers people who need support throughout self-isolation or self-quarantine by connecting them with state, local, and regional resources as necessary, such as food and housing. |
| DC | As of July 2022, the city has ended its universal contact tracing program. As of December 2021, people can also self-report their positive COVID-19 test result in the DC COVID Alert Notice (DC CAN) app, which is expected to help DC Health more quickly identify and notify close contacts. People who take a rapid, at-home test are asked to report their results to DC Health online. The District released guidance for businesses, community establishments, and public events. Health care facilities are required to provide contact tracing data to DC Health within 12 hours of the data being requested. |
| DE | In March 2022, the state launched a text messaging system to contact positive cases and provide initial isolation recommendations. A contact tracer may also contact positive cases after the text notification. Positive cases are recommended to follow the most current isolation guidelines and notify their own close contacts. Anyone within six feet of a person with COVID-19 for a cumulative 15 minutes in a 24-hour period is considered a contact. Positive cases or confirmed contacts who need extra support to self-quarantine (e.g., grocery delivery or alternative housing) are referred to a network of local community health workers coordinated by Healthy Communities Delaware. |
| FL | In January 2022, the state recommended that county health departments cease contact tracing. The state recommends that those with COVID-19 tell their close contacts about their exposure. The state recommends that residents contact their local health departments via phone or email to report results of at-home tests. |
| GA | The state conducts initial contact tracing outreach via manual calls to positive cases. Phone calls or text messages are sent to contacts of positive cases, who are then enrolled in symptom monitoring. Contact tracers assess people’s needs and connect them with a care resource coordinator to get them support to help with isolation or quarantine. Anyone within six feet of a person with COVID-19 for at least 15 minutes, starting two days before they became sick, is considered a contact. As of January 2022, and in response to omicron, some counties prioritize high-risk cases in congregate settings. |
| HI | In April 2022, the state ended its universal contact tracing effort. The state recommends that people use home test kits, follow self-isolation guidelines, and notify their own contacts when positive. The state focuses on cases in long-term facilities and schools and also encourages those who have tested positive for COVID-19 to alert their own close contacts. Anyone who was within six feet of someone while they were contagious for 15 minutes or longer over a 24-hour period is considered a contact. |
| ID | The state conducts initial contact tracing outreach via manual calls to positive cases and their contacts. Anyone within six feet of a person with COVID-19 for at least 15 minutes over a 24-hour period is considered a contact. In September 2021, districts launched a COVID-19 data collection tool for self-reporting positive test results. Central District Health prioritized contact tracing for people who are at higher risk, schools with populations at increased risk for COVID-19, congregate living facilities, long-term care residents, and people unable to receive the vaccine. |
| IL | As of June 2022, all positive cases in the state’s data system associated with a phone number receive an automated text message from the Illinois Department of Public Health (IDPH) providing information about resources, isolation guidelines, and close contact notification. Individuals will also be directed toward resources in multiple languages. The state will no longer make individual case investigation calls but will continue case notification for all confirmed/probable COVID-19 cases. The state will continue investigations of cases in congregate facilities and focused interventions. |
| IN | The state shifted away from universal contact tracing to a cluster or outbreak-based model. Individuals can confidentially notify their close contacts using www.tellyourcontacts.org. Anyone who was within 6 feet with a COVID-19 infected person for a cumulative 15 minutes over a 24-hour period is considered a close contact. Indiana law requires prisons and other congregate settings to report positive cases to the state department of health and conduct contact tracing. |
| IA | The state no longer conducts contact tracing for every COVID-19 case. Instead, contact tracing and case investigation focuses on outbreaks and populations at greater risk for exposure to COVID-19. The state does not contact schools or employers about positive cases, though localities may continue this work. As of January 2022, some counties have ended their contact tracing programs. When conducting tracing efforts, the state conducts initial contact tracing outreach via manual calls to positive cases and their contacts. Contact tracers offer to set up services, such as grocery deliveries, and share advice on how to safely social distance or quarantine. |
| KS | The state no longer conducts case investigation and contact tracing, citing high caseloads and resistance to participation. However, if the individual with COVID-19 exposed others at high-risk settings such as schools, correctional facilities, shelters, day-care facilities, and churches, state and local health departments will notify the setting. The setting will be responsible for identifying close contacts and notifying them about the potential exposure. The state Department of Health and Environment advises prisons to screen inmates, staff, and visitors for COVID-19 and requests all cases be immediately reported to the Health and Environment’s Epidemiology Hotline. |
| KY | As of March 2022, the state no longer conducts universal contact tracing except among people at higher risk of potential exposure to COVID-19. Some local health departments are shifting away from individual contact tracing and focusing on congregate settings or people at higher risk of potential exposure to COVID-19. |
| LA | The Louisiana Department of Health is no longer conducting case investigation and contact tracing of individual cases of COVID-19 but continues to investigate COVID-19 outbreaks and cases in high-risk settings. In March 2022, the Louisiana Department of Health launched a COVID-19 Support Hotline that combined an existing contact tracing hotline and a vaccine information hotline. Individuals who test positive for COVID-19 may receive a text message with general information on isolation and quarantine guidance. Individuals who test positive or suspect they have been exposed to COVID-19 and have questions may call the COVID-19 Support Hotline. Through the COVID-19 Support Hotline, the Community Support Team can give guidance for isolation and talking to close contacts as well as connection to a Community Health Worker, who may be able to assist with food, personal protective equipment, prescription delivery, housing, and utilities assistance. |
| ME | As of February 2022, the state no longer conducts contact tracing due to the rapid spread of the omicron variant and a backlog of positive tests. The state health department recommends that individuals who test positive for COVID-19 notify their own close contacts. |
| MD | The state conducts initial contact tracing outreach via manual calls to high-priority positive cases and their contacts. Those who test positive at home are encouraged to follow up with a test at a pharmacy or other testing site to allow for formal capture by the state Department of Health. Otherwise, individuals should notify their close contacts, self-report their results via their at-home kit mobile app, and/or contact their local health department to report their positive result. |
| MA | In December 2021, officials decided to end the state’s contact tracing program in favor of more testing and vaccine outreach. Residents are encouraged to use MassNotify, the state’s exposure notification app. As of July 2022, the Contact Tracing tab was removed from the state COVID-19 data dashboard. Local health departments have been advised to only do tracing in higher-risk settings, such as nursing homes, homeless shelters, and schools. Although some departments have opted to continue contact tracing most cases until it becomes overwhelming, others have opted to cut back. Local boards of health, with assistance from epidemiologists, conduct extensive investigations and contact tracing if clusters of cases emerge in long-term care facilities and nursing homes. |
| MI | Local health departments are advised by the state to focus contact tracing efforts on congregate settings, including schools, long-term care and assisted living facilities, and prisons. The state will call from MI COVID HELP or send a text. Statewide contact tracing and individual-level case investigation efforts have ended, but local health departments may continue these efforts. Case investigations within outbreaks informs a public-facing outbreak reporting tool. |
| MN | In October 2021, the state Department of Health announced changes to the contact tracing policy. Those diagnosed with COVID-19 are sent an online survey; contact tracing shifted to surveillance of targeted groups that can inform policy, including pediatric cases, breakthrough cases, hospitalizations, and new variants. As of May 2022, the state was reportedly no longer conducting contact tracing. As of January 2022, the state asks those who test positive with an at-home test kit to reach out to their own close contacts. The state has contact tracing guidelines for congregate settings, including shelters and drop-in centers. |
| MS | The state has not provided detailed information about its contact tracing work conducted by the department of public health. |
| MO | In April 2022, the state shifted from universal contact tracing to encouraging local contact tracing for people at greater risk for exposure to COVID-19. In December 2021, the state attorney general sent a letter to schools and local health departments (LDHs) ordering compliance with a court ruling that struck down regulations giving LDHs the power to impose COVID-19 public health orders. Some responded by stopping all COVID-19 related work, including case investigations and contact tracing, whereas others have requested to appeal the ruling. |
| MT | In May 2022, the Montana Department of Public Health and Human Services announced it would scale COVID-19 reporting back to weekly and that local public health officials would continue to investigate COVID-19 outbreaks and cases in settings that may expose individuals at high risk for severe outcomes. Anyone within six feet of a person with COVID-19 for at least 15 minutes in the two days before onset of symptoms is considered a contact. Some local jurisdictions are transitioning away from universal case investigation and contact tracing to focus on priority populations such as people who are at higher risk and people in congregate settings. Some county health departments—such as Missoula, Gallatin, Ravalli, and Lewis and Clark—use automated contact tracing and case investigation. Health departments follow up with email or calls for people without texting capability if the online form is not completed within three days. In July 2022, the City-County Health Department reported it was discontinuing contact tracing for COVID-19. |
| NE | In December 2021, the state Department of Health and Human Services (DHHS) changed its contact tracing procedures due to more infectious variants. Case investigators and contact tracers in some jurisdictions now focus on large clusters rather than individual cases. In addition, positive cases or contacts may receive a text message from DHHS asking them to complete a survey. Nonresponders may receive follow-up via phone call. Through the survey, positive cases can identify their close contacts and receive information on how to isolate. Once DHHS receives the completed survey, it notifies the identified close contacts, providing them guidance on how to quarantine. |
| NV | In February 2022, the state health department announced that individuals who test positive for COVID-19 should inform their own close contacts. The state conducts initial contact tracing outreach through calls to positive cases and their contacts. Contact tracers provide information and resources. Anyone within six feet of a person with COVID-19 for at least 15 minutes is considered a contact. As of January 2022, the Washoe County Health District added a case investigation self-service survey, sent via text message, to positive cases 18 and older. The health district also began sending automated text messages and emails to notify close contacts. |
| NH | The state conducts initial contact tracing outreach via phone calls to positive cases and their contacts. The state also tracks vaccine status of reported cases as part of its contact tracing efforts. As of June 2021, the state no longer conducts contact tracing for exposures in community settings but does investigate suspected outbreaks. The state recommends that long-term care facilities and assisted living facilities follow Centers for Medicare & Medicaid Services and CDC guidelines. |
| NJ | As of May 8, 2022, the state is no longer conducting contact tracing for the general population, and individuals who test positive are encouraged to get in touch with their own close contacts. Contact tracing is still being performed at long-term care facilities, in schools, and in other congregate settings. |
| NM | The state conducts initial contact tracing outreach via manual calls to positive cases and their contacts. The state provides interpreters in their contact tracing efforts. The state’s COVID-19 Toolkit, updated in June 2022 recommends that individuals who test positive for COVID-19 notify their close contacts. Restaurants are required to keep logs of customers for contact tracing purposes. Businesses also participate in surveillance testing and contact tracing with the Department of Health to avoid closures. Essential businesses can avoid mandatory closures if they regularly test employees and help with state contact tracing efforts. |
| NY | On April 28, 2022, the state ended its contact tracing program. As of winter 2021/2022, the state is following CDC’s case investigation and contact tracing guidance, which focuses on providing information to those who tested positive most recently and those who may have close contacts in sensitive settings. In January 2022, the state gave local health departments the ability to suspend contact tracing for COVID-19, as public health staff focus on testing, vaccination, case investigation, and special settings. Some local jurisdictions may continue contact tracing. In New York City, universal contact tracing ended in April 2022, but tracing will continue in high-risk congregate settings. NYC’s Health and Hospitals Corporation launched a COVID-19 Quarantine and Isolation Guidance Tool to assist those who have tested positive. The tool includes connections to resources, including free meal and care package delivery, testing, and treatment. |
| NC | The state conducts initial contact tracing outreach primarily via text or email to positive cases and their contacts. In some circumstances, they may reach out via calls. The state Department of Health and Human Services (NCDHHS) prioritizes calls for those associated with outbreaks or living/working in high-risk settings, such as congregate living facilities. Additionally, NCDHHS prioritizes calls to people who did not receive a text or are part of under-resourced communities. Anyone within six feet of a person with COVID-19 for at least 15 minutes is considered a contact. |
| ND | The state conducts initial contact tracing outreach via manual calls to positive cases and their contacts. Contact tracers focus on identifying clusters of COVID-19 cases. The North Dakota Department of Health links to CDC guidance for childcare, workplaces, and businesses. The state has moved away from contacting businesses of positive cases and providing return to work letters for employees following COVID-19 isolation. In February 2022, the state released updated recommendations for long-term care, basic care, and assisted-living facilities, which include performing contact tracing to identify any health care providers who have had a higher-risk exposure or residents who may have had close contact with an individual who tested positive for COVID-19. |
| OH | In January 2022, the state recommended that local health departments shift from universal contact tracing to a cluster- or outbreak-based model. Because local health departments are no longer contacting every positive case, the state created isolation/quarantine guidelines for the general public. |
| OK | In January 2022, the state announced it would move away from universal case investigation and contact tracing amid the omicron surge. Instead, they will focus on outbreaks and clusters in high-risk settings. The state encourages the public to conduct their own case investigations and contact tracing through a state self-service case investigation system. Case investigations involve two automated surveys—a risk assessment and abbreviated survey covering recent travel, hospitalization, and vaccination status. Contact tracers are still available by phone to complete interviews or answer questions. Participating individuals will receive downloadable letters to give employers or schools as well as information on how to quarantine and/or isolate. |
| OR | In March 2022, the state announced it was ending contact tracing and quarantine for the general population, including in schools. The state has investigative guidelines that recommend contact tracing only during investigation of high-consequence outbreaks. These settings include, but are not limited to, long-term care facilities, adult foster homes, child and adult behavioral health facilities, residential treatment facilities, intellectual and developmental disabilities 24-hour residential programs, carceral settings, homeless shelters, temporary/ transitional housing, K-12 and early learning settings, other congregate living settings (e.g., employer-provided communal housing, supported/supportive living), and agricultural and food chain facilities (e.g., farms, packing houses, processing facilities) |
| PA | The state has prioritized contact tracing to populations considered most at risk and cases that could lead to greater community spread. Community health nurses provide information on isolation, asymptomatic transmission, and how to monitor symptoms. Contact tracers notify individuals who may have been exposed in congregate settings and follow up with the respective facilities where the congregation took place. Contact tracers are also playing a large role in educating individuals. Contact tracing at long-term care facilities is conducted by individual county health departments. In Philadelphia, when case counts regularly exceed approximately 250 cases a day, the health department may not be able to reach out to every case and contact for contact tracing. The city provides guidance for individuals to notify their own contacts |
| RI | In February 2022, the state began to focus case investigation and contact tracing response efforts on people who are at higher risk and outbreak detection, with the intention of shifting away from universal contact tracing. The state health department prioritizes robust outbreak detection and response in pre-K through grade 12 settings and focuses case investigation efforts on people at high risk of serious disease, including people aged 60 and older, unvaccinated people, and people aged 45 and older in high-density communities. The state conducts initial contact tracing outreach through phone calls to positive cases and follows up with close contacts through text messaging. The state has expanded its online results portal, which allows contact information for their close contacts. The state’s text-based contact tracing system will then notify contacts, providing further instructions and guidance. |
| SC | The state is no longer conducting universal case investigations and contact tracing. The state Department of Health and Environmental Control recommends that positive cases notify their own close contacts. The state is now prioritizing cluster outbreaks involving populations in high-risk, congregate settings with the potential risk of ongoing transmission—e.g., people living or working in congregate living facilities (nursing homes, assisted living, correctional facilities, high-density workplaces, or other settings with potential ongoing transmission.). |
| SD | The state uses text messaging or email to conduct initial contact tracing outreach. These messages ask contacts to log on to a secure online portal where they can provide additional information. Contacts receive daily texts asking about symptoms if they enroll in the text message system. Anyone within six feet of a person with COVID-19 for at least 15 minutes over a 24-hour period is considered a contact. |
| TN | The state and local departments of health are scaling back contact tracing. They are no longer conducting universal contact tracing and are instead focusing on high-risk settings such as nursing homes, prisons, and homeless shelters. The state defines a close contact as someone within 6 feet of an infected person for a total of 15 minutes or more or shared direct physical contact with an infected person. The Jackson-Madison County Regional Health Department is focused on outbreaks in high-risk settings such as long-term care facilities and shelters, and will send positive cases isolation guidance through text message. The Metro (Nashville) Health Department is contact tracing when outbreaks arise in high-risk settings, including schools. |
| TX | In September 2021, the state budget prohibited funds from being used for contact tracing. Local health departments decide if and how to conduct contact tracing. For example, the Houston Health Department reaches out to positive cases by phone, automated email, or automated text messages. |
| UT | As of March 2022, the state announced Utah’s COVID-19 response would transition to a “steady state.” Most people will only get a text message from Utah public health after they test positive or are exposed to COVID-19 instead of a phone call. The department of health is prioritizing calling people who test positive or are exposed to COVID-19 and who live or work in settings where the risk of spread is very high, like a long-term care facility or detention center. The health department will also prioritize calling people if they are part of a large outbreak, like at a worksite or school. As of January 2022, the state encourages people to notify their own contacts, in response to a surge use of at-home test kits. |
| VT | As of January 2022, the state is no longer contacting every positive case. The state recommends infected individuals reach out to their own close contacts. The state continues to conduct contact tracing in long-term care facilities and shelters. |
| VA | In January 2022, the state announced that it will only conduct contact tracing in high-risk settings and in follow-up of an outbreak. The state recommends that individuals notify their close contacts and provides guidance to help them do so, including a link to a website where people can text or email close contacts anonymously. When conducting case investigation and contact tracing, contact tracers place manual calls to individuals who test positive, along with their contacts. The state may also notify positive cases via a series of automated text messages, which include a link to the new COVIDWISE Verification Code Portal. This allows those who have tested positive to submit their results to the COVIDWISE app for exposure notification. During outreach, contact tracers also attempt to enroll cases into the SARA Alert system. This software is used to conduct symptom monitoring through text or email. The contact tracer will provide education, information, and support to help those who might have been exposed. |
| WA | In March 2022, the state shifted from universal contact tracing to focusing on four key areas: outbreak investigation, case investigations in high-risk settings, targeted case investigations among those at risk of more severe illness, and targeted case investigations among those with unusual illness presentation. The state recommends that individuals with COVID-19 notify their own close contacts.Those who used an at-home test can request a verification code through the WA Notify app to anonymously alert other WA Notify users who may have been exposed. The state conducts initial contact tracing outreach to positive individuals and their contacts, usually by phone. The state department of health also has a toll-free number for people to report their at-home test result to assist with contact tracing. Anyone within six feet of a person with COVID-19 for at least 15 minutes over a 24-hour period is considered a contact. The University of Washington (UW) sends a workplace or classroom notification with recommendations to UW community members who were close contacts with an infected individual at a UW location. |
| WV | As of February 2022, the state’s Department of Health and Human Resources Bureau transitioned from universal case investigations and contact tracing to targeted case investigations and outbreak investigations. The state health department website provides guidance for individuals who test positive for COVID-19, including isolation and notification of close contacts. |
| WI | In January 2022, the state Department of Health released a memo encouraging local and tribal health officials to prioritize case investigation and contact tracing on preventing transmission to people at a higher risk. Contact tracing is no longer expected for every positive case but should be used for high-risk settings. Some counties have targeted certain age groups for contact tracing, due to the state’s memo, the omicron surge, and staff shortages. Other counties are ending contact tracing altogether. When it is conducted, contact tracing outreach takes place via manual calls to positive individuals and their contacts. As of October 2021, contact tracers from the state department of Health Services and local and tribal health departments can notify close contacts by sending a text or email. Contact tracers offer recommendations for quarantining and sign people up for self-monitoring. They can also connect people with isolation facilities. The state requires the reporting of outbreaks of COVID-19, and of facility-wide investigations. A contact is anyone who had direct physical contact with the positive case, was within six feet for more than 15 minutes over a 24-hour period, had contact with the person’s respiratory secretions, or had direct physical contact. Those who cared for, lived with, or stayed overnight for at least one night in a household with a positive case are also considered contacts. |
| WY | As of March 2022, the state health department is no longer attempting to reach individuals who have tested positive for COVID-19 unless they are part of a high-risk congregate settings such as long-term care facilities and correctional facilities, outbreaks and clusters of related cases, and the emergence of new variants. The state is no longer routinely issuing isolation and quarantine orders for COVID-19. Some counties are continuing to contact positive cases, prioritizing those who are in high-risk settings or who have increased risk. |
| State | CICT in K-12 Schools |
| AL | The state updated guidance for schools in August 2022, linking to the updated CDC guidance for schools, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. Schools are required to report outbreaks of COVID-19 to the state department of health using a Communicable Disease Report Card. |
| AK | The state provides guidance to schools based on CDC recommendations. |
| AZ | The state released guidance for summer camps in June 2022, including instructions for contact tracing. It also provided a link to the CDC guidance for schools, updated in August 2022, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. |
| AR | The Arkansas Department of Health links to the August 2022 CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. As of February 2022, Arkansas public schools are no longer requiredto contact trace or quarantine students who are exposed to someone with coronavirus. Schools may decide to continue contact tracing. The state Department of Health continues to investigate positive cases at schools and day-care facilities for those who are 18 and under. |
| CA | In January 2022, the state released updated guidance for schools to transition to a group-tracing approach for students exposed to COVID-19 in a K-12 setting. Per legislation approved in March 2021, schools are required to report COVID-19 cases to their local public health department, which will conduct contact tracing. Schools should have a COVID-19 liaison to assist the local public health agency with contact tracing. In June 2022 the state released updated guidance for schools for the 2022-2023 school year. The state recommends that schools notify students who spent more than a cumulative total of 15 minutes in a shared indoor airspace with someone with COVID-19 during their infectious period. In lieu of individual exposure notifications, the state recommends that schools consider providing a general notification to the entire school community during times of elevated community transmission of COVID-19. |
| CO | The state’s August 2022 guidance recommends that schools and childcare facilities continue to alert students, staff, and parents of known classroom cases, outbreaks, and exposures in lieu of individual case investigation and contact tracing. Quarantine for routine classroom exposures is not recommended unless it is part of a mitigation strategy put in place by the school, district, or local public health agency when cases are increasing, outbreaks are detected, or community levels are rising. In September 2021, the state issued an order requiring the department of education to provide the state health department with student data to match names in the state’s vaccine database. As of July 2022, the state department of health will stop publicly reporting COVID-19 outbreak data at K-12 schools, instead processing the data more similarly to flu outbreak data. |
| CT | The state health department’s fall 2022 guidance for schools, childcares settings, and camps recommends that schools use COVID-19 prevention strategies based on the CDC COVID-19 community transmission levels. Facilities in counties with a High COVID-19 Community Level can consider implementing advanced mitigation, including universal masking and contact tracing, to prevent further surges or outbreaks at their facilities. Schools are required to report all cases to the state department of public health. Schools are also encouraged to share general information about COVID-19 cases in their facilities with families. |
| DC | DC Health’s guidance for schools and childcare facilities released in June 2022 recommends carrying out contact identification when a case of COVID-19 is identified and dismissing potential close contacts; facilities should have a process in place to notify individuals who may have been exposed to COVID-19 at the facility; and contact identification should focus on COVID-19 cases who started having symptoms or tested positive for COVID-19 in the last five days and contact notification should focus on those who were exposed in the last five days. In January 2022, the DC Council passed a bill requiring public schools to notify parents within 24 hours if a student in their child’s class tested positive for COVID-19. |
| DE | The state recommends that schools and childcare facilities follow CDC guidance on COVID preventive measures, which include contact tracing if a school or program is experiencing a COVID-19 outbreak. |
| FL | As of January 2022, some counties suspended contact tracing in schools and have instead shifted to notifying families of students when a positive case happens in their child’s classroom and encouraging them to follow quarantine procedures. Other counties continue to contact trace with a focus on clusters instead of individual cases. The state recommends that during outbreaks, schools and childcare programs should inform those who may have been exposed if they identify a positive case. |
| GA | For the 2022-2023 school year, the state defers to CDC guidance for schools, which recommends that schools or childcare programs experiencing a COVID-19 outbreak should consider adding prevention strategies regardless of the COVID-19 Community Level, including case investigation and contact tracing. The state created a K-12 Public Health Liaison position at the Department of Education to work with the DPH on school health issues. This role includes ensuring efficient and expedited testing, contact tracing, data collection, reporting, and supports for COVID-19 in school settings. The state recommends cohorting in childcare facilities to limit the number of children, teachers, and staff who come in contact with each other and to assist in contact tracing. Childcare programs are advised to collaborate with the local health district and DPH on contact tracing efforts for children, teachers, and staff. |
| HI | The state’s COVID-19 school guidance for the 2022-2023 school year states that schools should conduct group notification to staff and families of students when exposed to a person with COVID-19 as soon as possible. When there is a suspected or a confirmed cluster, schools should notify all impacted staff and families as soon as possible to recommend testing at least twice following exposure, with one of the tests taking place on day 5. |
| ID | The state Department of Education provides guidance for schools to conduct their own contact tracing, based on CDC guidance. Schoolsconduct contract tracing for cases identified at school. Central District Health has a school exposure form for families, students, and staff to report positive tests and their close contacts. |
| IL | As of August 2022, the state fully adopted the CDC Operational Guidance for K-12 Schools and Early Care and Education Programs to Support Safe In-Person Learning. This guidance states that schools experiencing a COVID-19 outbreak should consider adding prevention strategies regardless of the COVID-19 Community Level, including case investigation and contact tracing. . |
| IN | As of February 2022, the state Department of Health no longer recommends that schools conduct contact tracing. Schools no longer need to report COVID-19 case information to the state. |
| IA | The state does not require schools to conduct case investigation or contact tracing. |
| KS | State and local health departments notify people about outbreaks at schools, despite the end of the statewide case investigation and contact tracing program. The state’s guidance for the 2022-2023 school year reflects CDC’s guidance for schools. The state recommends that, during an outbreak, schools consider strategies that can help reduce transmission, which include case investigation and contact tracing. To communicate exposures, schools may consider posting a list of classrooms and extracurriculars and the date(s) of exposure or push notifications to parents. |
| KY | In August 2022, the state updated its guidance to schools, stating that contact tracing following school exposures to COVID-19 is not expected. The state recommends that, where feasible, schools should notify families and staff when a known exposure to COVID-19 occurs in the classroom or in school settings. |
| LA | In July 2022, the state health department released updated contact tracing guidance for schools, indicating that contact tracing remains a critical step to control the spread of COVID-19. Schools should identify close contacts of persons identified as having COVID-19 and notify them of the need to quarantine. If both the case and the contact were consistently and correctly using well-fitting face masks and were at least three feet from each other, then those close contacts do not need to quarantine. As of February 2022, schools with universal mask mandates are not required to conduct contact tracing. |
| ME | As of February 2022, the state suspended recommendations for contact tracing in schools. In August 2022, the state announced that Maine adheres to the CDC’s Guidance for COVID-19 Prevention in K-12 Schools. The state’s summary document notes that quarantine is no longer recommended for people who are exposed to COVID-19 in schools. Vaccinated students who are traced in the University of Maine system are exempt from quarantine requirements. |
| MD | In July 2022, the state released updated guidance for schools in line with CDC school guidance. Universal contact tracing is no longer recommended in schools and childcare programs. When a COVID-19 case has been identified at any Community Level: The individual with COVID-19 (or their parents) should be encouraged to notify their own/their child’s close contacts; schools and childcare programs should provide notification of the COVID-19 case to the school or childcare community at the cohort level; close contacts, regardless of their vaccination status, can continue to attend school and childcare as long as they remain asymptomatic. Mask wearing for 10 days is recommended, as is testing at 3-5 days after exposure. Based on local conditions, schools and childcare programs may elect to perform universal or targeted contact tracing and quarantine of close contacts per CDC quarantine guidance. Contact tracing and quarantine are recommended in response to an outbreak. |
| MA | In August 2022, the Department of Public Health announced that contact tracing is no longer required in childcare, K-12, out-of-school time and recreational camp settings. Schools or programs should continue to work with their Local Board of Health in the case of outbreaks. Universal mask requirements, surveillance testing of asymptomatic individuals, contact tracing, or test-to-stay testing in schools are not recommended. Quarantine is no longer required or recommended for children or staff in these settings, regardless of vaccination status or where the exposure occurred. |
| MI | The state refers schools to the CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. |
| MN | The Minnesota Department of Health refers schools to the CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. The state has reporting mechanisms in place to schools and childcare programs to report cases of COVID-19. |
| MS | The Mississippi State Department of Health released guidance in July 2022 recommending that K-12 schools follow the CDC Guidance for COVID-19 Prevention in K-12 Schools as the primary guideline for establishing processes to prevent COVID-19 transmission in the school setting, and to maintain safe in-person education. |
| MO | The state’s guidance for the 2022-2023 school year refers schools to the CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. The state provides an antigen testing program, available to all schools. |
| MT | The state adheres to the CDC’s exception to the close contact definition. The Montana Department of Public Health and Human Services linksto the August 2022 CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. |
| NE | The state contracted with Professional Research Consultants, a health care research company, to conduct contact tracing for schools. |
| NV | In February 2022, the state health department updated guidance for schools, stating that masked contacts in a K-12 setting would no longer be considered exposed, regardless of distancing. |
| NH | The state links to the August 2022 CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. Schools and childcare facilities should report weekly aggregate COVID-19 datato the state. If a large cluster or outbreak is suspected, or if a school/childcare official is concerned about uncontrolled transmission within a facility, the school or childcare program can contact the state health department to report the situation and seek advice on mitigating further spread of COVID-19. |
| NJ | The state released updated guidance for schools in July 2022, recommending that schools provide broad-based notification to families, students, teachers, caregivers, or staff about a potential exposure in lieu of universal contact tracing. The guidance indicates that in the context of an outbreak, individual-level contact tracing, exclusion, and/or testing may be needed to prevent further transmission. In January 2022, the state Department of Health released Test to Stayguidance for schools, which specifies that asymptomatic students designated as a close contact of a student who tested positive can remain in school if they test negative. The state tracks COVID-19 in-school outbreaks, defined as three or more cases linked through contact tracing. |
| NM | The state’s toolkit for schools, updated in July 2022 covers required surveillance testing and protocols to facilitate contact tracing such as cohorting. |
| NY | In August 2022, the state departments of health and education announced that schools should follow the August 2022 CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. This update removed the recommendation for test-to-stay and the daily COVID-19 case reporting requirement for schools. |
| NC | In August 2022, the state department of health announced that schools should follow the August 2022 CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. Universal contact tracing is no longer recommended. |
| ND | The North Dakota Department of Health links to the August 2022 CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. |
| OH | As of January 2022, the state announced that K-12 schools may discontinue universal contact tracing but are expected to assist local health departments with outbreak or cluster investigations within schools. Schools are required to report positive cases to the local health departments weekly. |
| OK | In July 2022, the state health department released updated guidance for schools based on CDC guidance. Universal case investigation and contact tracing are not recommended, but they can used in responding to a school outbreak. |
| OR | Schools are responsible for creating their own communicable disease plans for the 2022-2023 school year. In March 2022, the state announced it was ending contact tracing and quarantine for the general population, including in schools. |
| PA | In August 2022 the state health department provided updated guidancefor schools based on CDC guidance, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. Schools are encouraged to report positive cases to the state health department on a weekly basis. The health department will continue to provide testing and vaccination support to schools, as well as public health consultation on outbreaks or a rapid rise in cases. |
| RI | In August 2022 the state released updated guidance for schools based on updated CDC guidance, recommending case investigation and contact tracing as one of the extra steps schools can take during a COVID-19 outbreak. Schools should notify the state health department when there are outbreaks. |
| SC | The state released guidance for schools on responding to COVID-19 outbreaks in July 2022. The guidance indicates that schools should identify close contacts during outbreaks. Outbreaks should be reported to the regional health department. The state health department also links to the updated CDC guidance for schools, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. |
| SD | The state links to the August 2022 CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. |
| TN | The state’s August 2022 guidance for individuals with COVID-19 and close contacts indicates that schools may adopt response strategies and policies for illness consistent with their needs for maintaining safe operations. In February 2022 Metro Nashville Public Schools announced that rather than tracing close contacts, classrooms will be notified as a whole if there is a positive case, along with guidance on how to monitor for symptoms and when they are recommended to get tested for COVID. |
| TX | The state’s guidance for schools released in August 2022 does not address contact tracing. Contact tracing was not required for schools in the 2021-2022 school year. |
| UT | As of August 2022, the Utah Department of Health and Human Services recommends schools implement a layered COVID-19 prevention approach consistent with the Utah COVID-19 Disease Plan and CDC school guidelines. In September 2021, the state began using an automated contact tracing for students in grades 7-12, sending text or email notifications to parents or guardians with a link to a questionnaire. This is a temporary change until the caseload lightens. Schools are required to do a Test to Stay event within 14 days of 2% of students testing positive in schools with 1,500 or more students. As of December 2021, the state has linked databases of positive COVID-19 cases with the state K-12 enrollment databases to better identify the location of outbreaks. |
| VT | Updated guidance for schools from the state departments of health and education released in August 2022, do not mention contact tracing. Testing is only recommended for symptomatic students and staff. |
| VA | The state’s updated guidance for schools, released in August 2022, does not address contact tracing. Quarantine is no longer routinely recommended for asymptomatic individuals after exposure to COVID-19 infected individuals. As of January 2022, the state no longer requires schools to conduct universal contact tracing. |
| WA | The state released updated guidance for schools and childcare programs in August 2022, confirming that contact tracing and quarantine after exposure are not required. Schools and childcare providers are required to have a process in place to inform students, children, and their families when there are cases and outbreaks in the school or childcare facility, which can include weekly newsletters or online dashboards of cases and outbreaks or group notification. All cases, outbreaks, and suspected outbreaks are required to be reported to the local health jurisdiction. |
| WV | The state’s updated guidance for schools, released in August 2022, indicates that universal contact tracing is not required. Schools are required to report cases in aggregate to the state weekly. |
| WI | State guidance for schools, updated in August 2022, indicates thatuniversal case investigation and contact tracing are no longer recommended and that the focus is now on outbreak prevention. Quarantine periods are omitted; asymptomatic individuals may continue to attend school after exposures. The state supports broad-based efforts to notify people of a potential exposure in schools while noting that exceptions to this approach may be required to protect students and staff at higher risk of complications of COVID-19. The state suggests that districts inform their school community of the chosen notification approach. |
| WY | The state links to the August 2022 CDC guidance for school settings, which recommends case investigation and contact tracing if the school or childcare program is experiencing a COVID-19 outbreak. When identification of specific close contacts is not possible because of resource constraints, such as at high levels of transmission, notification should be made to any group with potential exposure, such as a classroom or a team. |
| State | Workforce and Training |
| AL | |
| AK | In January 2022, the state reduced its contact tracing staff in response to its new testing strategy and omicron’s fast rate of transmission. |
| AZ | |
| AR | |
| CA | In July 2022, Los Angeles County reported having 100 contact tracers. |
| CO | The state maintains a contact tracing team to support local governments and partner organizations that hire and manage their own teams. Local governments trained public workers and police in Denver to conduct contact tracing. The state hired AmeriCorps and Senior Corps members and deployed the Colorado National Guard to support the state’s COVID-19 response, including contact tracing. A volunteer group of public health professionals, the Colorado Public Health Workforce Collaborative, supports local public health agencies by recruiting and training a contact tracing workforce, monitoring the rollout of contact tracing, and facilitating complementary containment activities. |
| CT | In January 2022, it was reported that Connecticut’s contact tracing system, ContaCT, employed 242 tracers, 21 supervisors, and 19 community outreach specialists, along with 132 volunteers. The state partners with the Community Emergency Response Teams to recruit volunteers. |
| DC | |
| DE | In May 2020, the state contracted with NORC at the University of Chicago to hire and train contact tracers and scale up technology. School districts have also helped conduct contact tracing and have closely partnered with their local health departments. Nurses are primarily responsible for documenting positive cases, contact tracing, and reporting to the state health department. |
| FL | |
| GA | |
| HI | In April 2022, the state said that contact tracers will return to other jobs. |
| ID | |
| IL | Chicago contact tracers include staff from local health departments, health care and community-based organizations, and schools. The Chicago Cook Workforce Partnership received funding from state and federal funds to conduct community-level contact tracing and has hired more than 800 people since the program was launched. The program has been extended through the end of 2022. The city has also allocated funding to partner with federally qualified health centers and hospitals for case investigation and contact tracing support through July 31, 2022. |
| IN | |
| IA | |
| KS | The state monitors virus hot spots and fills gaps at local health departments. In February 2022, the state began reassigning contact tracing staff to case investigation. |
| KY | Students from the University of Louisville have been involved with state and city contact tracing. In addition, the state has partnered with vendors to hire and train contact tracers. |
| LA | The state contracts with Accenture and Salesforce to manage the contact tracing process and create an electronic contact tracing platform. |
| ME | School nurses were Maine CDC’s primary point of contact for families and confirmed cases at schools. College athletic trainers were also contact tracers for student athletes, coaches, and staff. |
| MD | In January 2022, the state reported plans to hire 100 additional contact tracers, adding to a workforce of 700 state contact tracers and 400 others working at a call center. American Rescue Plan Act funds will support 100 contact tracing positions in Baltimore. The city ran a pilot for theBaltimore Health Corps to increase contact tracing capacity, as well as create jobs for trusted community members with racially equitable hiring and career development possibilities. With support from the Rockefeller Foundation, the Open Society Institute—Baltimore, and the Johns Hopkins Health System, the Baltimore health department expanded their workforce from 15 to 250 contact tracer positions. Due to staff shortages, Arundel County leaders focus contact tracing efforts in targeted areas such as childcare and assisted living settings. |
| MA | Contact tracing is conducted by local health boards. Student volunteers from schools of public health at the state’s colleges and universities participate in the Academic Public Health Volunteer Corps. |
| MI | Rock Connections manages volunteers, and Deloitte manages technology for the tracing program. In April 2022, the Michigan Public Health Institute announcedit would lay off 67 temporary workers. |
| MN | In December 2021, the Minnesota Department of Health (MDH) awarded AM LLC a service contract for opening and operating community pop-up testing sites throughout the state. AM will also process the test samples and report results to MDH and other interested parties. The firm also offers a range of COVID-19 prevention strategies and solutions for all COVID-19 mitigation phases, including contact tracing. Rose International provides support and hires staff on behalf of MDH. |
| MS | |
| MO | |
| MT | The state Public Health Training Center and Montana Department of Public Health and Human Resources offers a customized Contact Tracing Certificate course. The course aims to support local and tribal health departments with contact tracing. |
| NE | The state has worked with Professional Research Consultants, a health care research company, to provide contact tracing support to local health departments and school districts. The state also works with Nelnet and North End Teleservicesto staff contact tracing positions. |
| NV | |
| NH | |
| NJ | In March 2022, the health department said it plans to downsize its contact tracing workforce based on federal guidance that no longer calls for all cases to be investigated. The state developed a Community Contact Tracing Corps in partnership with the state’s higher education institutions and Public Consulting Group (PCG). Staff recruited by PCG are required to complete the contact tracing training developed with Rutgers School of Public Health. The Community Contact Tracing Corps also provides COVID-19 health education, testing, and contact tracing support to underserved groups, including Black and Latino communities. |
| NM | Navajo Nation has its own contact tracing program through the Community Outreach and Patient Empowerment (COPE), a Native-led nonprofit based in Gallup, New Mexico. It leverages an existing mobile app developed in partnership with Brigham and Women’s Hospital that was originally used to follow up with cancer patients. |
| NY | Bloomberg Philanthropies helped the state health department recruit potential contact tracers. The Johns Hopkins Bloomberg School of Public Health developed an online curriculum. The nonprofit Vital Strategies provides technical and operational advising. |
| NC | As of March 2022, the state no longer includes data on the contact tracing workforce on its dashboard. The state is part of the Carolina Community Tracing Collaborative, partnering with Community Care of North Carolina and the North Carolina Area Health Education Centers. These organizations work with Partners in Health to coordinate the contact tracing workforce in the local health departments. The state recruits those who are unemployed, have community engagement experience, and live in the communities that they serve. In collaboration with Community Care of North Carolina, the North Carolina Area Health Education Centers Program created an onboarding training curriculum that local health departments can use to train volunteers and other staff as contact tracers or case investigators. |
| ND | Contact tracers include some public health graduate students who are receiving course credit and volunteers of the Medical Reserve Corps. Lutheran Social Services is assisting with contact tracing efforts for people who speak English as a second language. |
| OH | |
| OK | |
| OR | The Oregon COVID-19 Contact Collaborative is a joint contact tracing effort with Oregon Health Authority, local health authorities, health districts, tribal authorities, and community-based organizations (including advocacy and community health worker groups). Tracing Health, a program launched by a nonprofit called Oregon Public Health Institute, helps counties recruit and train contact tracers. Tracing Health uses a health equity approach that matches contact tracers with communities based on language. |
| PA | The state’s Department of General Services contracted with Public Consulting Group after terminating its contract with Insight Global due to a data breach. The National Guard also assisted. In Philadelphia, health department community nurses and the National Guard conduct contact tracing. The state created the Commonwealth Civilian Coronavirus Corps, which bolsters local and community contact tracing efforts. Regional consortiums assess the number of contact tracers needed in each area of the state and recruit more staff and coordinate efforts accordingly. |
| RI | The state is carrying out its contact tracing efforts in partnership with the National Guard and using a platform created by Salesforce. Pharmacy and medical students are also involved. |
| SC | Contact tracers are trained by Johns Hopkins School of Public Health and the Association of State and Territorial Health Officials (ASTHO). The South Carolina Area Health Education Consortium (AHEC) helped to tailor these trainings for the state. In June 2021, Piedmont Technical College offered a contact tracing course it developed in collaboration with the state Department of Health and Environmental Control. Those who complete the four-week course receive an ASTHO contact tracing certificate. |
| SD | The University of South Dakota’s Community Action Response Epidemiology (CARE) team has partnered with the state to conduct contact tracing. The CARE team includes current health sciences undergraduates, recent graduates, and faculty members. |
| TN | The Metro Public Health Department replaced 50 contact tracers with an automated messaging platform called Teletaskwith the goal of using savings to add staff to the county’s vaccine rollout. |
| TX | In September 2021, the state budget prohibited funds from being used for contact tracing. The state no longer provides staff to assist with contact tracing. Two counties worked with local universities to increase their staffing. One county is also working with Texas A&M University School of Public Health’s Department to develop a larger increase in their pool of epidemiologists. Another county is working with the University of North Texas to recruit 90 students as part-time contact tracers. UT Health Austin’s contact tracing department does contact tracing for UT Austin students and works with Austin Public Health to support contact tracing broadly. |
| UT | In March 2022 the Utah National Guard ended its mission supporting the state with COVID-19 testing, vaccinations, contact tracing, logistical and medical support, and operational planning after two years. Navajo Nation also has its own contact tracing programthrough the Community Outreach and Patient Empowerment (COPE), a Native-led nonprofit. Their program leverages a mobile app developed in partnership with Partners In Health and Brigham and Women’s Hospital. |
| VT | In March 2022, the state’s contractor AM had 40 workersdedicated to contact tracing in Vermont. The state hired 9 new staff in anticipation of taking over contact tracing internally when the AM contract ends. The state relies on a rapid response team made up of Health Department staff and state partners to conduct contact tracing in long-term care and group living settings. The governor established the Vermont Enhanced Testing and Tracing Task Force that includes experts from the Department of Health and agencies affiliated with the Human Services and Digital Services, to monitor technological and workforce needs. |
| VA | Multiple universities have taken on contact tracing for their respective campuses. The University of Virginia partnered with its local health district to fund seven new positions for contact tracing on campus. Virginia Commonwealth Universityand the state have partnered to form a campus contact tracing team. Virginia Tech has implemented a Case Management Team to assist with contact tracing and coordinating quarantining and isolation on campus. |
| WA | Spokane Regional Health District is contracting with the Public Health Institute for contact tracing and will continue COVID-19 contact tracing through 2022 with a focus on high-risk settings. |
| WV | In June 2022, the National Guard’s role in supporting the state’s COVID-19 response ended. The state health department also partnered with West Virginia University to develop an online class to train contact tracers and certify them through the Association of State and Territorial Health officials. |
| WI | The state created a State Emergency Operations Center to organize and train contact tracers and coordinate volunteers from the Emergency Assistance Volunteer Registry. The state awarded Health Connections Incorporated grant funding to provide targeted on-site testing, contact tracing, and mental health and basic needs assessments to African American persons in Milwaukee County. |
| WY |
| State | Technology |
| AL | In August 2020, the state launched the GuideSafe Exposure Notification App, which uses Bluetooth location technology designed by Apple and Google. The app was developed by the Birmingham-based tech company MotionMobs in collaboration with the state health department and the University of Alabama at Birmingham. The state has joined the Association of Public Health Laboratories’ National Key Server, which allows GuideSafe to download keys from other exposure notification apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| AK | In January 2022, the University of Alaska Anchorage launched the Alaska COVID ENX exposure notification system, which uses Bluetooth location technology designed by Apple and Google. The state has joined the Association of Public Health Laboratories’ National Key Server, which allows GuideSafe to download keys from other exposure notification apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| AZ | The state implemented a secure, automatic symptom monitoring and reporting system, SARA Alert, that enables cases and contacts to report symptoms daily by phone, text, or online. Contact tracers record data for contacts of positive cases using a Qualtrics survey tool. The state released Covid Watch Arizona, an anonymous exposure notification app,which is a joint project of the University of Arizona and WeHealth that uses Bluetooth technology developed by Apple and Google to log Bluetooth signals of other nearby users. The state joined the Association of Public Health Laboratories’ National Key Server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. The state’s largest COVID-19 testing labs, Sonora Quest and Labcorp, no longer use the app to send verification codes to users. In July 2021, the state ended its digital contact tracing program, but the app is still available for download. |
| AR | The state uses the Situational Awareness Response Assistant (SARA) Alert system for case management. This system flags cases with reported symptoms for follow-up by Arkansas Department of Health (ADH) staff. ADH also uses SARA Alert to identify specific areas to target for testing and to provide information to support the state’s decision making. |
| CA | The state uses an app developed by Dimagi to manage contacts and texts for people to report symptoms. The state partnered with Accenture to launch a system using Salesforce and Amazon Connect for case management. The state uses the Virtual Assistant, an automated system from California Connected. The system sends texts with a link to chat with the Virtual Assistant, and can also provide contact tracing surveys, FAQs, and a symptom-monitoring system. The state launched CA Notify in December 2020. The app detects whether participants were near someone with COVID-19 via Bluetooth. As of December 2021, the system has reportedly been activated on over 15.6 million devices. The state allocated $4 million to the app. An estimated 160,000 users who tested positive have used the system to alert others. The CA Notify app is part of the Association of Public Health Laboratories’ National Key Server, which allows it to download keys from other exposure notification apps that are on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| CO | The state uses an online symptom tracker. The state uses a mobile service application in partnership with Google and Apple called CO Exposure Notifications. The app uses Bluetooth to sense whether a user’s device has been within six feet of someone who has tested positive for COVID-19 for a total of 15 minutes or longer in a given period. As of December 2021, over 3 million people have downloaded the app. The state is a participant in the Association of Public Health Laboratories’ National Key Server. The state’s exposure notification app can download the keys or codes of any other state’s exposure notification app if they are both participating. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| CT | The state uses, ContaCT, a statewide, voluntary software platform to automate some steps in the contact tracing process. Surveys are sent daily by email or text to people who have tested positive for COVID-19 and to people who were exposed. The tool also assesses unmet needs, such as access to food, housing, or health care, to connect people who are being asked to isolate with resources. The state uses Google and Apple’s exposure Bluetooth notification app, COVID Alert CT. If a user tests positive, a contact tracer asks the case to share the “close contact” codes. If the user agrees, those who met the close contact criteria for the app will receive an alert notifying them that they were a close contact of an anonymous case. The state’s exposure notification app is on the National Key Server, which allows apps to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| DC | The health department added new features to its technology system for managing contact tracing information, including logging individuals’ location and time of activities. This allows possible clusters of cases to be identified. In September 2020, DC rolled out an app based on Exposure Notification Express created by Apple and Google. The app allows users to receive notifications if they’ve been exposed to another user who tests positive for COVID-19. Users can self-report a positive test on the app. As of November 2021, 1,337,726 people had opted in to the official exposure notification system. DC is a participant in the Association of Public Health Laboratories’ National Key Server. DC’s exposure notification app can download the keys or codes of any other state’s exposure notification app if they are both participating. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| DE | As of March 2022, the Delaware Division of Public Health Contact Tracing Team uses a text messaging system to contact individuals who test positive for COVID-19. Individuals are asked for their birth date to confirm their identity but are not asked additional personal information. A member of the contact tracing team may contact individuals afterward for follow-up. The state worked with NORC’s technology partner, Enovational, and the Delaware Health Information Network to build a platform that enables the state health department to share data with contact tracers and Maryland. In September 2020, the state launched an app, COVID Alert DE, that uses Bluetooth technology to alert users that they have come in contact with someone who has tested positive for COVID-19. The state will discontinue the app on September 6, 2022. The state is a participant in the Association of Public Health Laboratories’ National Key Server. The state’s exposure notification app can download the keys or codes of any other state’s exposure notification app if they are both participating. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| FL | Contact tracers use the Merlin system, which is the state’s repository of disease case reports. It includes people who recently tested positive and can automatically notify staff of high-priority cases. In April 2020, the state launched theStronger Than C-19 community action survey. The anonymous survey is designed to gather information that helps the state track COVID-19 to improve the distribution of resources and initiatives across the state. The state uses the Healthy Together mobile app for contact tracing. Use is voluntary and relies on location and Bluetooth data. Several counties use the exposure notification app CombatCOVID, which notifies users if they have come into contact with someone who has COVID-19. |
| GA | Contact tracers notify contacts and ask them to log their symptoms into an online monitoring platform. The platform was developed for the state by the technology services company MTX Group, using Google Cloud data. Georgia Tech uses the NOVID exposure notification app, which uses Bluetooth technology to send exposure alerts to contacts. The app is voluntary for students, faculty, and staff on campus. |
| HI | Since April 2020, the state uses a cloud-based platform developed by HealthSpace to monitor symptoms. People being monitored enter information about their health status. The state uses two local apps called AlohaSafe Story, which uses GPS technology to log the user’s location, and AlohaSafe Alert, which anonymously records contacts through Bluetooth and Google/Apple Exposure Notification technology. The state also participates in the Association of Public Health Laboratories’ National Key Server. The state’s exposure notification app can download the keys or codes of any other state’s exposure notification app if they are both participating. As of June 2022, 24 states and Washington, DC, have joined the National Key Server. |
| ID | The state uses the Situational Awareness Response Assistant Alert system for case management. People can choose to report symptoms daily via text, email, or phone call. Those with reported symptoms are flagged for follow-up by contact tracers. |
| IL | The state launched the Illinois Contact Tracing Collaborative, a technology-based strategy for all local health departments with three components: disease-reporting software, common management platform, and an app for use by COVID-19-positive patients and their contacts to get the services that they need. The Illinois National Electronic Disease Surveillance System sends an automated message through the Salesforce platform to all confirmed or possible cases. An automated address matching process can identify outbreaks for case investigation. |
| IN | |
| IA | The state contracted with DOMO to launch new contact tracing software in November 2020. |
| KS | In June 2020, the state passed a law prohibiting data collection through cell phone tracking, specifying that participation in contact tracing must be voluntary. The law was in effect through May 2021. |
| KY | The state employs an online tracking system that uses the Salesforce platform for case management. As of August 2020, the state rolled out GovConnect Contact Tracing software as a comprehensive case management system for COVID-19. |
| LA | The state uses Accenture and Salesforce for case management. The state uses a COVID-19 tracing app called COVID Defense. The free app uses Bluetooth technology to send exposure alerts to contacts. The Louisiana Department of Health’s Contact Tracing program uses SMS text messaging to provide COVID-19 positive individuals, their contacts, and travelers to the state with public health guidance and social services support while quarantined. In September 2021, researchers at Louisiana State University released the GeauxTrace app, which uses a smartphone’s Bluetooth technology to alert those who have been in proximity to people who have positive test results for COVID-19. The state also participates in the Association of Public Health Laboratories’ National Key Server. The state’s exposure notification app can download the keys or codes of any other state’s exposure notification app if they are both participating. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| ME | The state uses the Situational Awareness Response Assistant (SARA) Alert system for case management. The tool, developed by MITRE, enables the state to track and monitor cases. People report symptoms daily through web, text, email, or calls, which helps the state coordinate and direct care where it is most needed. The state Centers for Disease Prevention and Control sends text messages to individuals who test positive for COVID-19. Individuals must opt in to receive the text messages. |
| MD | A contact tracing platform called covidLINK helps collect information about people who test positive for COVID-19 and close contacts. The platform also incorporates medical data from the Chesapeake Regional Information Center for Patients. In January 2022, state health officials reported plans to roll out a web survey for infected residents to complete so contact tracers can quickly identify people who are most at risk of severe illness or are in locations where rapid transmission is likely. The state is a participant in the Association of Public Health Laboratories’ National Key Server. The state’s exposure notification app, MD COVID Alert, can download the keys and codes of any other state’s exposure notification app via Bluetooth Low Energy (BLE) technology if they are both participating. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| MA | The Commonwealth Health Insurance Connector Authority created a virtual support center. Accenture and Salesforce implement support center capabilities. Salesforce helps capture data from case investigations and contact tracing. Data from Salesforce are uploaded to MAVEN, the state disease surveillance system, daily. Testing facilities also report cases and contact info to MAVEN. The state uses the MassNotify App, which builds on Apple and Google’s automated exposure notification platform using Bluetooth technology. As of December 2021, 1.74 million people had enabled MassNotify. The state is a participant in the Association of Public Health Laboratories’ National Key Server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| MI | The state partnered with Deloitte to coordinate technology integration, such as an automated text messaging system to which people can opt into after the initial call with a contact tracer. The state uses MI COVID Alert, an app based on Apple and Google’s exposure notification platform using Bluetooth technology. The state is a participant in the Association of Public Health Laboratories’ National Key Server. The state’s exposure notification app can download the keys and codes of any other state’s exposure notification app if they are both participating. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. The Central Michigan District Health Department uses a secure text message notification system, TigerConnect, to inform individuals of positive COVID-19 results and begin contact tracing, allowing for streamlined and timely communication between positive cases and case investigators. The state Restaurant and Lodging Association produced two mobile applications to help restaurants meet state requirements for screening staff and collecting guests’ contact information. |
| MN | The state contracted with a private vendor for a computer system to implement contact tracing. HealthPartners and the University of Minnesota developed a mobile application called SafeDistance. Clinicians at HealthPartners are encouraging patients and the public in the Twin Cities area to use the application. In November 2020, the state launched COVIDAware MN, an app that notifies people when their phone has been near the phone of a person with COVID-19 for enough time to be considered a close contact. The state is a participant in the Association of Public Health Laboratories’ National Key Server. As of June 2022, 24 states and Washington, DC, have joined the National Key Server. |
| MS | Some universities, such as the University of Southern Mississippi, use the Everbridge contact tracing app. |
| MO | As of February 2022, the MO/Notify exposure notification phone application, developed by Washington University was available to the public. The Department of Health and Senior Services manages the COVID-19 Technology Response System. This includes the Electronic COVID-19 Case Reporting System, EpiTrax and Missouri’s Advanced Contact Tracing System (MO ACTS). The Electronic COVID-19 Case Reporting System allows medical providers and required reporting entities to enter positive case information. EpiTrax is a comprehensive disease surveillance system that receives reports from COVID-19 tests. EpiTrax uses test data to trigger case management and investigations by local public health agencies and DHSS staff. |
| MT | At least two county health departmentsuse SARA Alert, which allows individuals who have been diagnosed with COVID-19 or potentially exposed to the virus to report daily symptoms through web, text, email, and robocall. As of January 2022, the Flathead City-County Health Department and other health departments are conducting automated contact tracing using an online platform to contact those who test positive for COVID-19. These individuals are sent a link to a secure web-based survey to complete their case investigation; a case investigator follows up with those who do not complete the form within 24 hours. Missoula County uses PatientOne, a locally developed app, to help with case management of quarantined individuals. As of October 2021, residents who are cases or contacts are contacted with a text, rather than a phone call. Yellowstone County is using an unnamed software for trend identification of positive cases and contacts by health department staff. |
| NE | Information is entered into the Nebraska Electronic Disease Surveillance System, a database shared with the Centers for Disease Control and Prevention. The state uses “Text Nebraska,” an automated text messaging system, which sends a survey to positive cases and their identified close contacts. As of July 2022, the state continuing to promote the system to the public. |
| NV | The state uses the National Electronic Disease Surveillance System, which helps public health officials process, analyze, and share disease-related health information, including as it relates to contact tracing. The state also worked with Deloitte and Salesforce on a statewide digital contact tracing solution. Some counties struggled with the Salesforce platform. For that reason, Clark County began using EpiTrax. The state expanded EpiTrax use to other counties in the state. The state uses COVID Trace, an opt-in contact tracing app developed by Google and Apple that allows phones to anonymously exchange information when in close proximity through Bluetooth. The state has expanded capabilities of the COVID Trace app with Exposure Notification Express (ENX) through a partnership with Apple and Google. Now individuals can turn on ENX to alert users who have been within six feet for more than 15 minutes of a COVID-19 positive individual. The app is on the National Key Server,which allows apps to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| NH | |
| NJ | The state uses the Dimagi CommCare case management platform to centralize its contact tracing efforts. The state launched an exposure notification app, COVID Alert NJ, using Bluetooth proximity technology. As of November 2021, the state estimates that COVID Alert NJ has 3.5 million users. The app is based on the platform developed by Google and Apple. The app is on the National Key Server which allows apps to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| NM | The state is using communication and case management platforms developed by MTX Group, which identifies and follows up with potential cases over 14 days. Its modeling predicts where cases will grow and where more resources might be needed. Accenture manages the overall contact tracing effort and oversees privacy protections. The state also uses an exposure notification app called NM Notify, using Bluetooth proximity technology. The app allows individuals to manually input their positive home test results. NM Notify is on the National Key Server,which allows apps to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| NY | Contact tracers use a secure database developed by CommCare, a mobile data collection company, to track cases and monitor contact tracing efforts. New York City partnered with Salesforce to deploy a call center and case management system. As of February 2021, more than 1.3 million individuals have downloaded COVID Alert NY, the state’s exposure notification app. Based on technology developed by Apple and Google, the app is on the National Key Server which allows apps to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. NYC’s schools use digital platforms for attendance tracking to assist with contact tracing. NYC shifted to a text-based system in 2021 to reach close contacts and connect them to resources. |
| NC | The state uses the COVID-19 Community Team Outreach Tool, which allows people to enter their own symptoms and helps streamline contact tracing work across the state. The state uses an exposure notification app using Bluetooth technology, SlowCOVIDNC. As of September 2021, the app had been downloaded 938,845 times as of September 2021. The app is based on Google and Apple’s Exposure Notification System and alerts users if they have been in close contact with individuals who later test positive for COVID-19. The state targets marketing of the app to people at high risk of exposure to COVID-19, including colleges and universities. The app is also on the National Key Server which allows apps to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| ND | Previously, the Care19 Diary served as a memory aid that used location data to help users who test positive for COVID-19 recall where they have visited to assist the contact tracing process. The Care19 Alert app used exposure notification technology developed by Apple and Google for public health agencies to supplement their COVID-19 contact tracing efforts. The Care19 Alert app was on the National Key Server, but it has been discontinued. |
| OH | The state uses the Ohio Disease Reporting System. Some local entities, such as the Lake County school district partner with Volan Technology to use a Bluetooth-based contact tracing application. |
| OK | In November 2021, the state launched a new OSDH Case Investigation systemallowing the public to conduct their own case investigations and contact tracing. Although the Record Portal may be accessed on any device, a cell phone is needed for the initial registration process. The state is using an app created by Google and MTX Group that lets medical staff engage remotely with people who may have been exposed, directing those with symptoms to testing sites. In July 2021 the state reported it had updated its computer systems with new software from Google. |
| OR | In June 2021, the state passed a law that prohibits contact tracing apps and other websites from collecting, using, or disclosing personal COVID-19 public health data without express consent. |
| PA | The state is using SARA Alert, a web-based monitoring tool, to send daily emails, texts and/or phone calls to cases and identify close contacts during their isolation/quarantine monitoring period. The state has a digital contact tracing system called Connect and Protect that directs individuals (ages 19 to 64) who test positive to fill out an online contact tracing questionnaire. The state used an exposure notification app, COVID Alert PA, which used proximity exposure technology. Users could voluntarily report when they tested positive, which in turn anonymously alerted other phones that had been in proximity for a specified time. It was available in four languages. Individuals ages 13 through 17 were able to use the app with parental consent. As of July 2021, the App had 922,000 downloads. The app is on the National Key Server, which allows apps to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, have joined the National Key Server. As of July 2022, the state had plans to discontinue its exposure notification app in the coming months. |
| RI | The state uses Salesforce, a customer relationship management platform, to capture data from case investigations and contact tracing. The state has expanded its online results portal, which allows contact information for their close contacts. The state’s text-based contact tracing system will then notify the identified contacts, providing further instructions and guidance. The 401Health app shares daily location data for up to the past 20 days with the Department of Health, though the data are only made available if users opt in to sharing. The app also includes a symptom tracking survey. |
| SC | The state uses SCIONx (South Carolina Infectious Disease and Outbreak Network for Externals) for disease surveillance and outbreak management. The state Department of Corrections built an app to help track infections among prison staff. Clemson University uses the SC SAFER TOGETHER exposure notification app, which uses Bluetooth technology to notify users of a potential exposure. The app also provides steps to schedule a telehealth appointment, take a self-assessment, or schedule a test. The SC SAFER TOGETHER app was launched in collaboration with the Department of Health and Environmental Control, Clemson University, and the Medical University of South Carolina. |
| SD | The state Department of Health (DOH) provides a web-based questionnaire to aid in contact tracing. The DOH then notifies people identified as close contacts, with questions about their health and guidance on testing and quarantining. Together with North Dakota, the state uses Care19, a location-tracking app to map the spread of COVID-19 and assist with contact tracing. The Care19 app is a location-logging application for use in contact tracing. Use of the app and disclosure of location information is voluntary. |
| TN | The state uses the National Electronic Disease Surveillance System to facilitate communication between health care professionals and government agencies. In September 2021, the South Central Regional Health Office launched a text message COVID-19 case investigation system in conjunction with the state department of health. Residents of the region who test positive may receive a text message that asks them to complete their case investigation online and report their contacts. Traditional phone interviews will continue, but text messaging outreach is expected to accelerate traditional phone interviews for contact tracing. Sumner County schools notify parents through SchoolMessenger if a student in their child’s class tested positive. |
| TX | The City of San Antonio uses the emocha Health application to remotely monitor and support residents exposed to COVID-19. |
| UT | The state uses EpiTrax to manage positive cases and their contacts. In February 2021, Utah launched the Google/Apple Exposure Notification Express app. The app uses Bluetooth technology to log anonymous keys of other users’ nearby phones. If a user tests positive, they can send an alert to the phones they came in contact with through the app. The app is part of the National Key Server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| VT | The state is using the National Electronic Disease Surveillance System Base System to manage COVID-19 case data. This system helps public health departments manage reportable disease data and supports public health investigations. |
| VA | The state uses the Virginia Electronic Disease Surveillance System to contact and manage cases. This system is based on the Centers for Disease Control and Prevention’s National Electronic Disease Surveillance System Base System. The state also uses the SARA Alert system, which sends email and text messages that prompt a person with COVID-19 to complete a daily self-report of their symptoms. In May 2020, the state launched COVIDCheck, a website which allows people to check their symptoms and guides them to testing, if needed. The state also launched a proximity tracking app called COVIDWISE. Users must opt in to the COVIDWISE notification system which uses their phone’s Bluetooth technology to track other app users. If one user encounters another who had a positive COVID-19 test within the last 14 days, the app sends an exposure notification alert, along with next steps, from the Department of Health. COVIDWISE is a part of the National Key Server which allows it to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. In February 2021, the state launched COVIDWISE Express as an additional exposure notification tool for iPhone users. COVIDWISE Express does not require users to download the app but is activated through the Exposure Logging on their smartphone. |
| WA | The state uses the state’s notifiable conditions database, the Washington Disease Reporting System, to compile information about COVID-19-related test results. The state also uses a texting tool to send information to people quickly and efficiently. The state uses the WA Notify app, which is based on Google Apple Exposure Notification technology. Users can opt in to receive notifications if a contact tests positive for COVID-19. Users can also record positive results. As of August 2022, WA Notify had more than 3.53 million activations. The app is also on the National Key Server, which allows it to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| WV | The state uses the West Virginia Electronic Disease Surveillance System, a web-based electronic reporting system, for case management. |
| WI | The state uses the Wisconsin Electronic Disease Surveillance System, a secure system for entering, tracing, and monitoring information on active cases. The state launched the WI Exposure Notification app in partnership with Apple and Google. As of September 2021, 29% of residents have downloaded it. The app is on the National Key Server which allows it to download keys from other state apps on the server. As of June 2022, 24 states and Washington, DC, were part of the National Key Server. |
| WY | The state partnered with North Dakota-based ProudCrowd to create the Care19 Alert app, which was launched in North Dakota and South Dakota in April. The app keeps a record of a person’s location for potential use in contact tracing if the user then tests positive for COVID-19. Previously, the app is also on the National Key Server but it has since been discontinued. |
| State | Funding Allocated by State |
| AL | In June 2021, the CDC awarded the Alabama Department of Public Health over $40 million to address COVID-19-related disparities, including improving and increasing contact tracing among populations that are at higher risk and underserved. In March 2021, the CDC awarded a $29.6 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. Federal coronavirus relief money allocated to the state health department paid for the contact tracing contracts. The state received more than $30 million in CARES Act funding to provide testing, symptom monitoring, and notification of exposure to COVID-19 for higher education students in all of the state’s public and private institutions. |
| AK | In November 2021, the president announced an investment of $92 million from the Indian Health Service to hire school nurses that can provide contact tracing and other COVID-19 mitigation strategies, as well as $6 million to support core surveillance work for American Indian and Alaska Native populations. In June 2021, the CDC awarded $36 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $5.2 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. To develop a contact tracing curriculum, the University of Alaska Anchorage’s Center for Rural Health and Workforce accessed a $95,000 supplemental federal CARES Act grant, which the state matched. |
| AZ | The state paid $1.6 million to WeHealth Solutions to develop the Covid Watch Arizona app. In June 2021, the CDC awarded $34.6 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In May 2021, Arizona was given access to new federal funds of around $1.4 billion for Arizona counties and $1 billion for two dozen of the state’s cities to implement public health programming including services and programs to contain the spread of COVID-19, like contact tracing. In March 2021, the CDC awarded a $43.5 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. Maricopa County allocated $2 million in American Rescue Plan Act (ARPA) funds to support contact tracing and case investigation efforts. Pima County has spent roughly $15 million on case investigation and contact tracing from June 2020 until the end of January 2022. This includes $11 million from the federal CARES act and other grants. In November 2021, the Pima County Health Department received a $6.8 million grant to help ensure K-12 teachers and families have the resources needed to minimize the impacts of the pandemic, including continuing contact tracing among students and their contacts. |
| AR | In December 2021, the state awarded $4 million from federal CARES Act funding to the Arkansas Department of Health for COVID-19 case investigation and contact tracing. In June 2021, the CDC awarded $40.4 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded an $18.6 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The CDC awarded a $6 million grant to help employ 50 bilingual community health workers in Northwest Arkansas to help combat COVID-19 including placing them at contact tracing centers. |
| CA | In February 2022, Governor Newsom signed a $1.9 billion COVID package to bolster the state’s ongoing emergency response. Of these funds, $100 million will be used to support mutual aid, bolster contact tracing efforts, and procure personal protective equipment. As of January 2022, the state reported spending $259.3 million for contact tracing, with another $38.9 million going forward through the end of the next fiscal year. In June 2021, the CDC awarded $32.4 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing amongpeople who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded $173 million to the state and $59.7 million to Los Angeles County. This 2-year grant aims to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers, and prioritizes school-based health programs and local health departments. The American Rescue Plan Act (ARPA) provided $3.2 billion to the state for testing, contact tracing and other efforts to stop the spread of COVID-19. In 2020 the California Connected public awareness campaign launched with $5.1 million in funding, with partners including Jeff Skoll and his organizations, the California Health Care Foundation, The California Endowment, Twitter and Facebook, and other media partners. Universities provided contact tracing training through a state contract. |
| CO | In June 2021, the CDC awarded $22.5 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $34.6 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The Corporation for National and Community Service supported Colorado’s contact tracing initiative by redeploying AmeriCorps members and providing nearly $2 million in federal funding for new volunteers in August 2021. |
| CT | In June 2021, the CDC awarded $17.3 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $21.8 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state initially budgeted $23.8 million for the ContaCT system. |
| DC | In October 2021 the District allocated nearly $40 million to hire additional contact tracers, substitute teachers, and workers to handle COVID-19 logistics in schools ($20 million for public schools and $17 for local charter schools). In June 2021, the CDC awarded $5.1 million to the district health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved. In March 2021, the CDC awarded a $5 million, 2-year grant to the district to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| DE | As of October 2021, nearly $100 million has been allocated to the Health Care Relief Fund, which can fund contact tracing activities. In June 2021, the CDC awarded $24.5 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $6.7 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| FL | In June 2021, the CDC awarded $34.9 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing amongpeople who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $126.6 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state paid World Wide Technology of St. Louis $450,000 to design the Stronger Than C-19 community action survey to improve the distribution of resources and initiatives across the state. The state also contracted with Twenty Labs for the Healthy Together app. |
| GA | In June 2021, the CDC awarded $38.8 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $63 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| HI | In June 2021, the CDC awarded $24.5 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). University of Hawai’i’s Community Health Worker (CHW) program at Kapi’olani Community College, has received $313,000 to train additional contact tracers. In March 2021, the CDC awarded a $9.2 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state received $81 million for testing and contact tracing from the federal COVID-19 relief bill. The state will be using federal funding from the American Rescue Plan for testing, contact tracing, and vaccinations. |
| ID | The state is using $7 million from the CARES Act to fund contact tracers. In June 2021, the CDC awarded $30.7 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded an $11.4 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| IL | In June 2021, the CDC awarded $28.8 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). As of June 2021, local health departments across the state received approximately $230 million and community-based organizations received another $60 million. In March 2021, the CDC awarded a $59 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. Chicago awarded the Chicago Cook Workforce Partnership $56 million in state and federal funds to hire contact tracers and work with 31 community-based organizations to create a COVID Contact Tracing Corps and COVID Resource Coordination Hub. |
| IN | In October 2021, the Indiana Department of Health began offering funding to local health departments to support the hiring of personnel to assist schools with contact tracing and other response efforts. The funds, which come from two CDC grants, will be offered for two years, with $22.8 million available each year. In June 2021, the CDC awarded $34.8 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $40 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| IA | In June 2021, the CDC awarded $31.6 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $19 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state contracted with DOMO for $250,000 to develop new contact tracing software. |
| KS | The state Department of Health and Environment was awarded a federal cooperative agreement that includes $74 million to support local school districts’ COVID-19 mitigation strategies Blue Cross and Blue Shield of Kansas awarded a $200,000 grant to the Kansas Association of Local Health Departments, which passed through funds in $5,000 increments to local health departments across the state to support contact tracing efforts. In August 2021 the state health department was awarded over $1.7 million from the CDC to address health disparities and ensure access to COVID-19 services— including testing, contact tracing, and immunization services—and to improve community health resiliency. In June 2021, the CDC awarded $31.9 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded an $18 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| KY | In June 2021, the CDC awarded $42.8 million to the state cabinet for health. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). The state has a $4.27 million contract with Deloitte to oversee the contact tracing technology. A June 2021 report showed that the state spent $215 million of CARES Act funding on PPE, contact tracing, testing, and public awareness. In March 2021, the CDC awarded a $27 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state also receives Emergency Assistance to Non-Public Schools (EANS II) funding, which can be used for contact tracing. Nearly $290 million of the state’s share of the December 2020 Federal COVID Relief bill will be used for COVID-19 contact tracing, testing, and mitigation efforts. |
| LA | In June 2021, the CDC awarded $37.2 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In May 2021, the CDC Foundation gave Xavier University $420,000 to create strategies for combatting disproportionate rates of COVID-19 among African Americans in New Orleans. These strategies will include community outreach about contact tracing. In March 2021, the CDC awarded a $28 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| ME | In June 2021, the CDC awarded $32.1 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded an $8.8 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. In January 2021, the state’s congressional delegation announced receipt of an additional $89 million in federal COVID-19 relief funds, including $77 million for testing, contact tracing, and other strategies. |
| MD | In June 2021, the CDC awarded $21.2 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $36 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. In January 2021, the state’s congressional delegation announced receipt of over $400 million in federal funding from the Federal COVID Relief bill to expand COVID-19 vaccine distribution, contact tracing, and testing capacity. In October 2021, Baltimore announced that $80 million of American Rescue Plan Act funds would be used to address COVID-19. Some of the funds will support 100 contact tracers, making positions permanent for some of the existing tracing staff and allowing others to return to their original roles. Baltimore also received $25 million in response funding from the Harry and Jeanette Weinberg Foundation. |
| MA | In December 2021, the Massachusetts Department of Public Health announced it is awarding $12.6 million in community-based funding to fight COVID-19. It includes $8.6 million in school health workforce funds and $4 million for local health boards for contact tracing and case investigations. The state maintained a contract with Partners in Health through December 2021, costing roughly $158 million in total). The state replaced its contact tracing program to support local boards of health in the amount of $15 million from the Baker-Polito administration and $4 million from the state Department of Public Health. Boston Public Schools responded to parents’ complaints for better COVID safety in schools as cases continue to surge by announcing new funding for COVID prevention. Officials plan to spend an additional $3 million on expanding contact tracing and hiring more contract nurses. In June 2021, the CDC awarded $18.5 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $41 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state has a $39 million contract with Accenture and Salesforce to develop and manage software. |
| MI | In June 2021, the CDC awarded $31.8 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the governor signed legislation that included up to $555 million in federal funding for testing and tracing. In March 2021, the CDC awarded a $59 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. In August 2020, the state began what would be an $18 million contract with the Michigan Public Health Institute. The contract ended in May 2022. |
| MN | In June 2021, the CDC awarded $25 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In December 2021, Minnesota’s senators announced that the U.S. Department of Health and Human Services will provide more than $19.5 million in funding to more than 75 rural hospitals in the state for COVID-19 testing and mitigation efforts, including contact tracing. In March 2021, the CDC awarded a $39 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state legislature authorized $8 million to create the information technology system needed to track cases and their contacts and $3 million to hire a temporary employment agency to fill staffing gaps. The state has awarded several local and tribal organizations funding to conduct community-based pandemic efforts, including contact tracing. |
| MS | In June 2021, the CDC awarded $48.3 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing amongpeople who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded an $18 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state received $171 million to support testing, contact tracing, containment, and mitigation to monitor and suppress the spread of COVID-19 from the December 2020 Federal COVID Relief bill. |
| MO | In October 2021, the state released a toolkit for how local governments can use American Rescue Plan Act (ARPA) funding for public health initiatives like contact tracing. In June 2021, the CDC awarded $36 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). As of June 30, 2021, the state had allocated $11.8 million to contact tracing and tracking. In March 2021, the CDC awarded a $36 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| MT | In June 2021, the CDC awarded $33 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $7 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state earmarked $144 billion of ARPA funds for COVID-19 contact tracing and testing, awarded via grants to public health departments, with $18 million for testing and tracing in schools. |
| NE | In June 2021, the CDC awarded $29 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $12 million 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| NV | In December 2021, the state allocated $85.2 million to be sent to the statewide epidemiology laboratory to upgrade that operation and the contact tracing program In June 2021, the CDC awarded $32 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $19 million 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. In January 2021, the state awarded the University of Nevada – Las Vegas School of Public Health an additional $1.7 million to continue contact tracing efforts, in addition to an initial $3.4 million award for contact tracing in September 2020. |
| NH | In June 2021, the CDC awarded $25 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $9 million 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state allocated $100 million from the American Rescue Plan Act for vaccines, testing, contact tracing, and other coronavirus-related expenses. |
| NJ | In June 2021, the CDC awarded $25 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $53 million 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| NM | In June 2021, the CDC awarded $39 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded $13 million to the state. This 2-year grant aims to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers, and prioritizes school-based health programs and local health departments. The state established a $12.5 million contract with Accenture Healthcare Services to set up a call center for contact tracing. New Mexico also has a $7.5 million dollar contract with MTX for contact tracing. |
| NY | In June 2021, the CDC awarded $66 million to Health Research Inc., an agent for the State Department of Health. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded $66 million to the state and $49 million to New York City. This 2-year grant aims to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers, and prioritizes school-based health programs and local health departments. As of September 2021, New York City estimates $3 billion in costs for their Test and Trace Corps for FY2022, which will be covered by federal funds. As of March 2021, New York City reported its contact tracing budget for the current fiscal year and the next at $582 million. |
| NC | In June 2021, the CDC awarded $40 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $62 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| ND | In June 2021, the CDC awarded $31 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $5 million 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| OH | In January 2022, the Ohio Department of Mental Health and Addiction Services released $2.98 million in ARPA funds for contact tracing and other COVID-19 prevention efforts. In June 2021, the CDC awarded $31 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $69 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| OK | In June 2021, the CDC awarded $44 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded $23 million to the state. This 2-year grant aims to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers, and prioritizes school-based health programs and local health departments. The state allocated $21.7 million funds from the CARES Act for testing and contact tracing. |
| OR | In June 2021, the CDC awarded $34 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded $25 million to the state. This 2-year grant aims to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers, and prioritizes school-based health programs and local health departments. |
| PA | In June 2021, the CDC awarded $28 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded $66 million to the state and $10 million to Philadelphia. This 2-year grant aims to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers, and prioritizes school-based health programs and local health departments. In July 2021, the state’s Department of General Services approved a new $34 million contract with the Public Consulting Group. In August 2021, the state awarded Public Consulting Group an additional $9 million to rebuild its contact tracing program. Previously, the state had a $30 million contract with Insight Global for contact tracing. The contract ended following a data breach. The state contracted with NearForm Ltd. at $1.9 million to deploy and maintain the Covid Alert PA app. The state spends about $20 million annually on contact tracing. |
| RI | The 2021 Rhode Island budget included $180 million to cover COVID-19-related expenses, including contact tracing. In June 2021, the CDC awarded $20 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $7 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. As of January 2021, the Rhode Island Department of Health had received $70.4 million in federal funding, with $61 million supporting testing, contact tracing, and containment and mitigation efforts. |
| SC | In June 2021, the CDC awarded $34 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $31 million 2-year grant to the state, to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. In February 2021, the state legislature voted to allocate $200 million for COVID-19 efforts, including contact tracing. |
| SD | In June 2021, the CDC awarded $38 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $6 million 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. |
| TN | In June 2021, the CDC awarded $39 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $40 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state ended its $65 million contract with Xtend Healthcare in February 2022. |
| TX | In the 2022-2023 State Budget, lawmakers added a provision stating funds appropriated by this Act cannot be used for the purpose of COVID-19 contact tracing, effective September 1, 2021. In June 2021, the CDC awarded $39 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded $157 million to the state and $14 million to Houston. This 2-year grant aims to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers, and prioritizes school-based health programs and local health departments. |
| UT | The state spent $2.75 million on the Healthy Together app and will pay $300,000 per month for maintenance fees. In June 2021, the CDC awarded $24 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $20 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. In February 2022, the state released the K-12 School-Based COVID-19 Response Grant, which provides $202,343 per school district through June 30, 2023 for COVID-19 response efforts, including contact tracing. The funding is part of the $20 million grant received from CDC in March 2021. In January 2022, the Navajo Nation President authorized $567 million of American Rescue Plan Act funds to be used to provide individual stimulus payments to the Diné community. |
| VT | In June 2021, the CDC awarded $28 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $4 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. In April 2021, the state awarded $10 million contract to Applied Memetics LLC. The contract provides up to 75 full-time contract tracers and allows the state to scale up their contact tracing force as needed. As of March 2022, the state has already paid the company $15 million. |
| VA | As of December 2021, the state reported spending $270 million of federal funding on contact tracing programs over the course of the pandemic. In June 2021, the CDC awarded $27 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded $50 million to the state. This 2-year grant aims to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers, and prioritizes school-based health programs and local health departments. |
| WA | For the 2022 budget, Governor Inslee has proposed using $300 million of federal coronavirus relief funds to support COVID-19 mitigation activities such as contact tracing. As of September 2021, the state department of health is planning to spend $212 million over the next two years in pandemic response, including contact tracing and investigation. In June 2021, the CDC awarded $29 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $45 million 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. In February 2021, Governor Inslee signed a bill to provide $618 million for COVID-19 response, including contact tracing. |
| WV | In June 2021, the CDC awarded $30 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded an $11 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. The state will receive $103.1 million through the Coronavirus Response and Relief Supplemental Appropriations Act to expand testing and contact tracing. |
| WI | In September 2021, the state received $58.4 million from the American Rescue Plan Act to continue responding to COVID-19. These funds can be used for a variety of activities to stop the spread of COVID-19, including contact tracing. In June 2021, the CDC awarded $27 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded a $35 million, 2-year grant to the state to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers. The grant prioritizes school-based health programs and local health departments. In January 2021, the state announced $86 million in funding for local and tribal health departments to offset COVID-19 related expenses, including contact tracing. |
| WY | In June 2021, the CDC awarded $38 million to the state health department. The 2-year grant aims to reduce COVID-19-related health disparities and improve and increase contact tracing and testing among people who are at higher risk and are underserved (including people living in rural communities). In March 2021, the CDC awarded $4 million to the state. This 2-year grant aims to support activities to expand, train, and sustain a response-ready public health workforce, including contact tracers, and prioritizes school-based health programs and local health departments. |