Across the country, states are launching new payment models that reward quality, promote care integration, improve access, and address the social determinants of health (SDOH) in an effort to improve population health. One of these ground-breaking initiatives is Rhode Island’s Accountable Entity (AE) Program, created to improve the health of Rhode Islanders enrolled in Medicaid managed care plans.
Rhode Island’s program is designed to encourage Medicaid managed care organizations (MCOs) and providers to deliver more cost-effective care through value-based payments, improve coordinated care delivery, and focus on population health in ways that go beyond traditional clinical care. Rhode Island Health System Transformation Project Director Lauretta Converse and AE Program Director Deborah Correia Morales, members of National Academy for State Health Policy’s (NASHP) State Accountable Health Models workgroup, recently shared how their program is addressing SDOH during the first year of AE implementation.
Could you describe Rhode Island’s accountable entity program and how it fits into your managed care model?
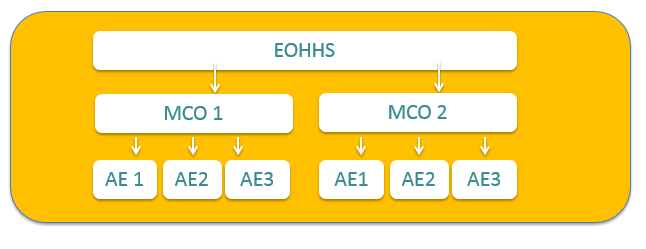
State officials developed the AE program through an amendment to the state’s 1115 Medicaid Demonstration Waiver as a way to move the existing Medicaid MCO model away from fee-for-service and towards value-based care to expand its ability to improve health outcomes and decrease costs. The AEs are provider organizations that once certified by the Executive Office of Health and Human Services (EOHHS ) are eligible to contract with one of the state’s MCOs. Specific contractual requirements set forth by the EOHHS provide guidelines for how MCOs and AEs should proceed in coordinating teams of providers with the goal of aligning financial incentives, improve their capacity to manage complex conditions, and better address social needs. The AEs, through increased delivery system integration and improved information exchange, will enhance the capacity of the MCOs and providers to support and serve high-risk populations. AE participation is voluntary, but once MCOs enter into an AE contract, they are eligible to receive incentive funding from a pool of total incentive dollars. During project Year 1, 15 percent of those dollars is allocated to the MCO incentive pool while 85 percent is allocated to the AE incentive pool.
How are you incorporating SDOH into the AE model?
AEs are accountable for care coordination for their attributed populations and are required to adopt a defined population health approach. Rather than having individual providers treat patients’ individual health issues one at a time, AEs coordinate a team of providers who take on increasing financial risk for treating the whole person. A central element of the AE model is the required integration of strategies to address SDOH. The strategies must include assessment of social needs, screening and referral to community resources, and using community partnerships and engagement to address identified needs. Rhode Island has taken this on through a three-legged stool approach: certification, payment, and incentives.
How certification works:
In the first year of the program, the EOHHS certified six AEs. The state’s EOHHS uses a set of certification standards that require:
- The identification of three key domains of social need
- Evidence of capacity to address those domains;
- A process for screening, managing referrals; and
- Arranging supports for patients who need them.
AEs work with their providers to identify the best points of contact with their patients, and are able to bring aspects of care management to a broader population. AEs must be able to demonstrate clear evidence of their capacity to address the three priority domains, which could be through defined relationships with community-based organizations, in-house social supports, or an agreement with a separate social supports agency.
Possible key domains include housing stabilization and support, education and literacy, food security, safety and domestic violence, employment, and transportation. As expected, the AEs all received conditional certification because they did not yet meet the necessary standards for providing services and supports from within the community or for screening and referring patients based on the SDOH [ ]. Rhode Island state officials recognize that the AEs need support, in this case in the form of incentive payments, to develop their capacity in this area and to reach the goal of emphasizing community-based resources and services in addition to institutional care.
How payment works:
Certified AEs participate in an EOHHS-designed, value-based, Alternative Payment Methodology (APM) and total cost of care (TCoC) model through contractual partnerships with MCOs. EOHHS contracts with MCOs, which then subcontract with the AEs, which makes the MCOs responsible for ensuring AE contractual compliance. These contracts are intended, over time, to move AEs away from shared savings to increased financial risk and responsibility and to move provider payments from volume-based to value-based arrangements. Payments to AEs, made by the contracted MCO, are based in part on the quality of the care they deliver to their members, as determined by the EOHHS Quality Scorecard, which includes an SDOH measure.
How incentives work:
AE infrastructure development and implementation are supported through the Health System Transformation Project (HSTP), an amendment to the state’s 1115 Medicaid Demonstration Waiver. Entering into APM contracts makes AEs eligible to receive incentive payments from their managed care partners, and AEs receive the funds in exchange for meeting milestones established by AEs and MCOs in an individualized HSTP plan. The milestones initially are based on infrastructure and capacity building and will transition to performance-based outcome metrics. well the AEs perform in accordance with the plan dictates the amount of incentive funding earned.
AEs are required to allocate 10 percent of their received incentive funds to establish partnerships between the AE and community-based organizations that support behavioral health care, substance abuse treatment, or SDOH. A key tenet of addressing SDOH is engaging with community supports so that relationships for referral, follow-up, and tracking are established. As such, it is a requirement of the program that the agreements between community partners and AEs be formalized along with the process of identifying partners’ specific service and referral needs.
How do AEs engage with community partners to help reach their goals and address social determinants of health?
EOHHS identified four steps for AEs to use to develop meaningful community-based partnerships in Rhode Island.
First, it is necessary to identify the appropriate partners to assist in addressing SDOH within a particular community. The next step is to formalize the agreement between the AE and the community partner to establish expectations and hold each party accountable for their responsibilities. The third step is to establish bi-directional care management tracking so that all parties, including the MCO, are as up-to-date as possible on the care of patients within the AE. Finally, partners develop metrics for measuring the SDOH efforts and need for any adjustments to maximize the impact of the partnership.
All of these steps are supported through a requirement that the AEs allocate 10 percent of their incentive funding to community-based organizations.
Why are social determinants so integral to new payment and delivery models?
An increasingly familiar statistic — only 20 percent of health outcomes are due to clinical health care — establishes the importance of addressing societal, behavioral, and environmental factors when attempting to improve health. Addressing SDOH not only improves the overall health of a community, it increases the capacity of a system to prevent poor health outcomes and to manage and treat the health needs of the people it serves. A payment and delivery model that holds providers accountable for the full range of factors that influence health outcomes is a model that is likely to decreases costs and improves results.
What are your next steps?
Thus far, AEs have identified housing, food, and domestic violence as their top social determinants. EOHHS hopes to see AEs increasingly engaged in addressing these issues in their communities while taking on additional financial risk and better meeting certification standards in Year 2 of the program.



